CLINICAL PROBLEMS AND CORRELATIONS
OF THE THORACOLUMBAR
SPINE
Low back pain, with or without leg pain, is very common in the population, particularly in middle-aged and older adults. Degeneration of the intervertebral disc and some degree of low back pain and stiffness are nearly universal features of aging. Degenerated discs have decreased height, increased posterior and lateral bulging, and reduced ability to dissipate compression forces. As a result, associated changes occur, including abnormal loading of the facet joints with development of facet arthritis, osteophyte formation, greater stress on adjacent ligaments and muscles, and thickening of the ligamentum flavum. In some patients, these changes may result in back pain, although it is difficult to isolate the primary source of low back pain in most instances. In some cases, back pain may become chronic. Chronic low back pain, defined as persistent symptoms for longer than 6 to 8 weeks, is common among people older than 40 to 50 years of age and those working in occupations requiring frequent bending, lifting, or exposure to repetitive vibration (e.g., truck drivers). Obesity, smoking, and poor physical fitness are all risk factors for disc degeneration.
A typical feature of back pain is its frequent radiation to one or both
buttocks. The pain can additionally radiate to the posterior thigh. It is
frequently exacerbated by lifting and bending activities and relieved with rest.
As with all chronic pain conditions, depression may aggravate symptoms and make
treatment more challenging.
 |
| DEGENERATIVE DISC DISEASE |
Examination typically shows mild tenderness in the lower back or
sacroiliac region. Flexion and extension of the spine may be limited and
painful. The straight-leg raising sign is typically absent, and findings of the
neurologic examination are normal. Patients with associated
psychological issues may display nonorganic findings, such as exaggerated pain
behaviors and non-anatomic localization of symptoms.
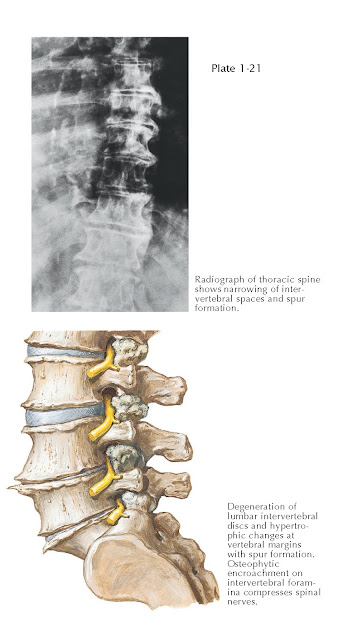
Radiographs and MR images of the spine reveal changes that are difficult
to differentiate from normal age-related changes. These include decreased disc
height, anterior vertebral body osteophytes, and decreased disc hydration (see Plate 1-21). Screening
radiographs to rule out tumor, infection, or an inflammatory arthritic process
are appropriate for patients with pain lasting
longer than 6 weeks. MRI should be reserved for patients with unusual symptoms
in whom an occult and sinister process is suggested, such as infection, tumor,
or fracture. It is also utilized as a diagnostic tool for patients with
unremitting symptoms in whom symptomatic nerve compression is suggested and who
are surgical candidates.
Recurrent episodes of back pain are typical, and most can be managed
nonoperatively with nonsteroidal anti- inflammatory drugs (NSAIDs), general
conditioning exercises,
active physical therapy, weight reduction, and smoking cessation. Unremitting
pain necessitates further evaluation. Operative treatment is rarely indicated
for back pain, and the role of fusion or arthroplasty for patients with
discogenic low back pain is controversial.
LUMBAR DISC HERNIATION
The nucleus pulposus may herniate posteriorly or posterolaterally and
compress a nerve root, resulting in lumbar radiculopathy (leg pain in a
dermatomal distribution). The herniation may be protruded (with the
anulus intact), extruded (through the anulus but contained by the
posterior longitudinal ligament), or sequestered (free within the spinal
canal). Pain results from nerve root compression and from an inflammatory
response initiated by various cytokines released from the nucleus pulposus (see
Plate 1-22).
Patients with lumbar disc herniation typically are young and middle-aged
adults with a history of previous low back pain. The pain may be exacerbated by
a bending, twisting, or lifting event but may also develop insidiously and
abruptly. The central portion of the posterior longitudinal ligament is the
strongest portion of the ligament and resists direct posterior extrusions. More
than 90% of lumbar disc herniations occur posterolaterally at L4-5 and L5-S1.
Posterolateral disc herniations may cause neural compression and radicular pain
involving the traversing spinal nerve. For example, an L4-5 posterolateral disc
herniation will typically affect the L5 nerve root. Occasionally, a disc
herniation will be located far lateral and can affect the more proximal exiting
nerve root within the foramen and can cause radicular pain
corresponding to the vertebral level cephalad to the disc (e.g., an L4-5 far
lateral disc herniation will affect the proximally exiting L4 nerve root).
Increasing pressure or stretch on the compressed nerve root exacerbates
pain. Pain can also increase with any activity that increases intra-abdominal
pressure, such as sitting, sneezing, and lifting. It is typically decreased by
lying down with a pillow under the legs or by lying on
the side with the hips and knees flexed (fetal position). Symptoms can be
variable, but pain and sensory disturbances typically follow the dermatome of
the nerve root(s) affected.
On examination, the patient may lean toward the affected side to relieve
compression on the affected root. The straight-leg raise test (lifting the leg
with the knee straight) is a classic sciatic nerve tension sign that indicates L5 or S1
root inflammation and should be performed on both legs. A positive test
typically reproduces the patient’s radicular symptoms below the knee. The
specificity of the test is heightened when raising the contralateral leg
provokes symptoms on the affected side (the cross-leg sign). The comparable
test for a more proximal lesion affecting the L4 root or higher is the femoral
nerve stretch test, which is performed by having the patient lie on the
nonaffected side and by having the examiner extend the affected hip with the
knee flexed. A positive test reproduces the patient’s proximal leg pain.
Radiographs of the lumbar spine may be normal but are useful in ruling
out other conditions such as fracture. MRI is the study of choice to delineate
the location and type of disc herniation. Most patients respond to symptomatic
treatment such as NSAIDs, muscle relaxants, oral narcotics, a short course of
oral corticosteroids, or epidural corticosteroid injection and will note
improvement of symptoms by 6 weeks.
Indications for surgery include cauda equina syndrome, urinary retention
or incontinence, progressive neurologic deficit, severe single nerve root
paralysis, and radicular pain lasting longer than 6 to 12 weeks. The goal of
surgery is to relieve pressure on the affected nerve root or cauda equina. The
procedure usually involves a small laminotomy and excision of the herniated
disc fragment (see Plate 1-22). Lumbar discectomy typically provides dramatic
relief of symptoms in 85% to 90% of patients. Recurrent disc herniations may
occur in 5% to 10% of patients. Possible complications of surgery include
injury to the neural elements, postoperative infection, durotomy, and
persistent pain.
CAUDA EQUINA SYNDROME
Multiple nerve roots of the cauda equina may be severely compressed by a
large central disc herniation or other pathologic process such as epidural
abscess, epidural hematoma, or fracture, resulting in a rapid onset of
neurologic deficit. Midline sacral nerve roots that control bowel and bladder
function are particularly vulnerable to such compression. Typical symptoms
include bilateral lower extremity radicular pain and motor/sensory dysfunction,
saddle anesthesia in the perineum, difficulty voiding, or frank bowel or
bladder incontinence. Patients with cauda equina syndrome require emergent
surgical decompression. Even with prompt treatment, however, the return of
neurologic function may be incomplete.

LUMBAR SPINAL STENOSIS (CONTINUED)
Lumbar spinal stenosis may result from any condition that causes
narrowing of the spinal canal or neural foramina with subsequent compression of
the nerve roots at one or more levels. The most common cause is degenerative
changes in the disc and facet joints. These degenerative changes are often
associated with a spondylolisthesis, which is an anterior slipping
(anterolisthesis) of one vertebra on the subjacent level. Patients with
achondroplasia or other conditions that alter growth of the posterior vertebral
arch may also develop stenosis with progressive symptoms in the second or third
decade of life. Lumbar stenosis may also be congenital or may be caused by
traumatic or post-operative changes.
Narrowing of the spinal canal is common in persons older than 60 years
of age, but most persons have minimal symptoms. The spine is a three-joint
complex comprising the intervertebral disc anteriorly and the two facet joints
posteriorly. It is thought that the pathology of spinal stenosis begins
anteriorly in the disc and involves the facet joints secondarily. Skeletal
changes associated with stenosis in the older population include disc bulging
and narrowing, degeneration and osteophyte formation of the facet joints, and, occasionally,
spondylolisthesis. Soft tissue changes associated with stenosis include
buckling or thickening of the ligamentum flavum and posterior longitudinal
ligament, as well as bulging or frank herniation of the disc.
Symptomatic lumbar spinal stenosis afflicts both sexes and typically
does not develop until after 40 years of age, unless there is a congenital
component. Typical symptoms include a diffuse pain in the buttocks and
posterior thighs or pain in a dermatomal and radicular pattern. Back
pain may or may not be present. Symptoms are frequently bilateral, but one
extremity may be more severely affected than the other. Patients note pain and
often numbness or weakness when walking, usually beginning in the buttocks or
thighs, and often progressing to the calves and feet. This condition is also
termed neurogenic claudication. Symptoms are typically relieved by
sitting, bending forward, or leaning on an object.
Forward-flexion of the lumbar spine reduces discomfort and improves exercise
tolerance by expanding the spinal canal, thereby relieving neural compression.
As a result, patients with symptomatic spinal stenosis sometimes walk with
their hips and knees flexed to allow for lumbar flexion (see Plate 1-23).
Patients typically report improved symptoms when leaning on a shopping cart,
walking up hills, or exercising on a recumbent bike, all of which permit a
slight degree of lumbar flexion, thereby relieving neural compression.
Vascular claudication may mimic neurogenic claudication and should be
ruled out because they may coexist. As with neurogenic claudication, patients
with vascular claudication may have increased leg pain with exercise that is
relieved by rest. However, patients with vascular claudication do not have pain
relief with lumbar flexion or walking uphill, have a fixed as opposed to
variable claudication distance, rarely have back pain, often have loss of calf
hair, and typically have diminished or absent peripheral pulses (see Plate
1-23).
Findings on examination are often limited in patients with spinal
stenosis. Lumbar range of motion may be either normal or diminished. Muscle
weakness, if present, is often subtle and may only be observed after having the
patient walk. Weight-bearing radiographs should be obtained and usually demonstrate
typical age-related changes of facet joint arthrosis, diminished disc height,
or a degenerative spondylolisthesis, most common at L4-5 and L3-4. The
differential diagnosis includes vascular claudication, peripheral neuropathy
associated with diabetes mellitus or vitamin B12 or folic acid deficiency,
abdominal aortic aneurysm, infection, and tumor.
 |
| DEGENERATIVE LUMBAR SPONDYLOLISTHESIS |
Nonoperative management is initially symptomatic and includes physical
therapy, NSAIDs, activity restriction, epidural corticosteroid injections,
weight reduction, and smoking cessation. Membrane-stabilizing agents such as
gabapentin have also been useful in reducing symptoms. When symptoms persist
and surgery is an option, diagnostic imaging with either MRI or CT
myelography should be performed. Weight-bearing lumbar radiographs are
mandatory, and flexion and extension lumbar spine views may also be useful to
rule out an associated degenerative spondylolisthesis. If spondylolisthesis is
present, decompression is usually accompanied by spinal fusion of the affected
levels. If no degenerative spondylolisthesis is present,
surgical therapy usually involves neural decompression alone.
Surgery is most effective to relieve leg symptoms of neurogenic
claudication. It is less successful in patients in whom back pain is the
predominant symptom and in patients with significant comorbidities such as
smoking, obesity, or diabetes. Surgical decompression of the stenotic level(s)
is usually palliative (see Plate 1-25). This is most
commonly achieved by a laminectomy, with foraminotomy as needed. Iatrogenic
instability can occur after complete removal of a unilateral facet joint, by
more than 50% facet resection bilaterally, or by removal of more than one third
of the pars interarticularis bilaterally. In such cases, a concomitant spinal
fusion should be considered. Recurrence of stenosis after decompression may
occur, particularly at adjacent levels to a concomitant spinal fusion.

DEGENERATIVE SPONDYLOLISTHESIS: CASCADING SPINE
DEGENERATIVE LUMBAR SPONDYLOLISTHESIS
Spondylolisthesis is translation (slippage) of one vertebra in relation
to an adjacent segment. The superior vertebra typically slips in an anterior
(forward) direction in relation to the inferior vertebra (anterolisthesis) (see
Plate 1-26). Retrolisthesis,
in which the superior vertebra slips posteriorly, can also occur. This is
occasionally observed in degenerative spondylolisthesis involving the upper
lumbar levels. The causes of spondylolisthesis vary, but the vast majority of
patients have either an isthmic or degenerative spondylolisthesis (see Plate
1-25). Isthmic spondylolisthesis typically occurs at L5-S1, begins during
adolescence, and is discussed elsewhere.
In degenerative spondylolisthesis (spondylolisthesis with an intact
neural arch), erosion and narrowing of the disc and facet joints lead to
segmental instability. Because the posterior arch is intact, the slippage
causes stenosis, which can be aggravated with flexion. This condition typically
occurs in adults past age 40, is more common in
women and blacks, and is most common at the L4-5 level. It can also occur at
other levels, however, and can result in the appearance of a “cascading spine”
(see Plate 1-26).
Symptoms include back pain, radicular pain, and neurogenic claudication.
Indications for surgical management include persistent claudicatory leg pain,
neurologic weakness, and, rarely, cauda equina syndrome. Because the affected
segments are unstable, decompression is usually
combined with fusion (arthrodesis). The addition of instrumentation improves
fusion rate. Decom- pression alone is associated with poorer outcomes than
decompression with concomitant fusion and may be associated with progression of
spondylolisthesis. It is therefore typically reserved for elderly, low-demand
patients with significant collapse of the disc and no motion detected on
flexion-extension lumbar radiographs.






