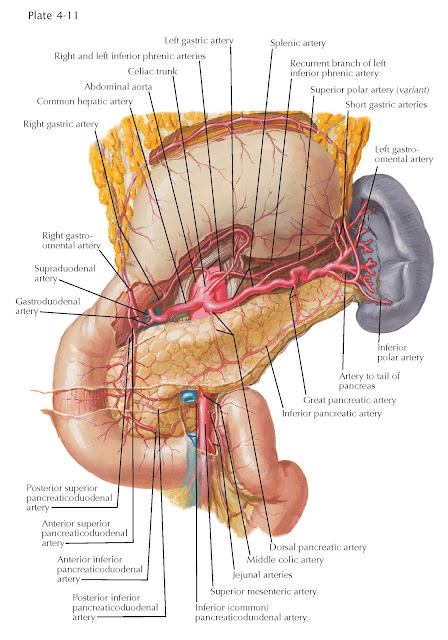
BLOOD SUPPLY OF
STOMACH AND DUODENUM
The conventional textbook description of the blood supply to the gastrointestinal organs and the spleen has established the misleading concept that the vascular patterns of these organs are uniform. In fact, they are unpredictable and vary in every instance. In the following account, we will first present the “typical” version of the vascular tree before examining the blood supply to each organ and then some of the common vascular variations that may be encountered in surgical resections.
Typically, the entire blood supply
of the foregut organs (liver, gallbladder, stomach, duodenum, pancreas, and
spleen) is derived from the celiac arterial trunk, a supplementary small
portion being supplied by the superior mesenteric artery via its inferior
pancreaticoduodenal branch. The caliber of the celiac arterial trunk varies
from 8 to 40 mm in width. Most typically, it gives off three branches, the left
gastric, common hepatic, and splenic arteries, which frequently have
the appearance of a tripod (25%).
 |
| ARTERIES OF STOMACH, LIVER, AND SPLEEN |
After branching from the celiac
trunk, the left gastric artery travels superiorly and to the left. It
reflects onto the cardiac region of the stomach and travels along the lesser
curvature of the stomach, travelling from left to right. It also gives off an esophageal
branch that ascends from the cardiac region of the stomach toward the
distal esophagus.
The common hepatic artery leaves
the celiac trunk and progresses to the right. In the vicinity of the portal
vein it divides, sending the proper hepatic artery superiorly. The right
gastric artery is also typically seen leaving this vessel and traveling to
the lesser curvature of the stomach, where it will anastomose with the left
gastric artery. As it travels superiorly, the proper hepatic artery divides
into right and left hepatic arteries, which travel into the liver.
Before entering the liver, the right hepatic artery most typically gives off
the cystic artery to the gallbladder. The other branch of the common
hepatic artery is the gastroduodenal artery. The small supraduodenal
artery, which travels to the superior duodenal flexure, most frequently
branches from the gastroduodenal artery. This vessel gives off the posterior
superior pancreaticoduodenal artery, anterior superior pancreaticoduodenal
artery, and, finally, right gastroomental (gastroepiploic) artery, which
travels along the right side of the greater curvature of the stomach.
The splenic artery, the celiac
trunk’s third branch, is a large, coiled artery that travels to the left of the
abdomen superior to, or within, the pancreas. It generally gives off a large dorsal
pancreatic artery to supply the head and body of the pancreas, along with
the greater pancreatic artery a bit further down its length. The artery
to the tail of the pancreas can be seen as a small branch of the distal
splenic artery connecting with the greater and dorsal pancreatic
arteries by means of the inferior pancreatic artery within the pancreas.
Near its terminus, the splenic artery gives off several branches that pierce
the hilus of the spleen to supply the organ. As this is happening, the short
gastric arteries leave the superiormost aspect of the splenic artery to
supply the fundus of the stomach. Inferiorly, the left gastroomental
(gastroepiploic) artery leaves the splenic artery to supply the left side
of the stomach’s greater curvature and anastomose with the right gastroomental
artery.
The blood supply of the stomach and
abdominal esophagus is accomplished by six primary and five secondary arteries.
The primary arteries are the (1) right gastric and (2) left gastric, coursing
along the lesser curvature; (3) right gastroomental and (4) left gastroomental,
coursing along the greater curvature (each of these four vessels giving off
branches to the anterior and posterior surfaces of the stomach, where they
anastomose); (5) splenic, which gives off in its distal third a variable number
(2 to 10) of short gastric branches, and from its superior or inferior
terminal division the left gastroomental; and (6) gastroduodenal, by direct
small branches (1 to 3) and, frequently, by a large pyloric branch.
The secondary arteries are the (7)
anterior superior pancreaticoduodenal (end branch of the gastroduodenal) by
short twigs and, frequently, by a large pyloric branch; (8) supraduodenal
artery of varied origin (gastroduodenal, posterior superior
pancreaticoduodenal, hepatic, right gastric) which, in addition to supplying
the first inch of the duodenum, often sends one or more branches to the
pylorus; (9) posterior superior pancreaticoduodenal, predominantly the first
collateral of the gastroduodenal, which, in its tortuous descent along the left
side of the common bile duct to reach the back of the pancreas and duodenum,
frequently gives off one or more pyloric branches, the latter, in some
instances, uniting with the supraduodenal and right gastric; (10) dorsal
pancreatic artery of varied origin (splenic, hepatic, celiac, superior
mesenteric), the right branch of which anastomoses with the superior
pancreaticoduodenal, gastroduodenal, and right gastroomental and, in so doing,
sends small branches to the pylorus; (11) left inferior phrenic, which,
after passing inferior to the esophagus in its course to the diaphragm, in most
instances gives off a large recurrent branch to the cardioesophageal end of the
stomach posteriorly, where its terminals anastomose with other cardioesophageal
branches derived from the left gastric, splenic terminals, aberrant left
hepatic from the left gastric, and descending thoracic esophageal branches.
This conventional form of the
celiac with its three branches occurs in only 55% of the population, for the
celiac often lacks one or more of its typical branches. Whether in a complete
or incomplete form, the celiac trunk forms a hepatosplenogastric trunk in about
90% of the population. The celiac may omit the left gastric, so that a
hepatosplenic trunk is present (3.5%); omit one or more of the hepatic
arteries, so that a splenogastric trunk is present (5.5%); or omit the splenic,
so that a hepatogastric trunk is present (1.5%). Additional branches may
originate from the celiac trunk: the dorsal pancreatic (22%), inferior phrenic
(74%), and, occasionally, even the middle colic or an accessory middle colic
artery. In many instances the common hepatic artery is absent, being replaced
from the superior mesenteric, aorta, or left gastric.
 |
| ARTERIES OF LIVER, PANCREAS, DUODENUM, AND SPLEEN |
Typically, the left gastric
artery arises from the celiac (90%), most commonly as its first branch. In
remaining cases it arises from the aorta, the splenic or hepatic artery, or a
replaced hepatic trunk. Varying in width from 2 to 8 mm it is considerably
larger than the right gastric, with which it anastomoses along the lesser
curvature. Before its division into anterior and posterior gastric branches,
the left gastric supplies the cardioesophageal end of the stomach, either by a
single ramus that subdivides or by two to four rami given off in seriation by
the main trunk. Accessory left gastric arteries occur frequently. They are (1)
a large left gastric from the left hepatic; (2) a large ascending posterior
gastroesophageal ramus from the splenic trunk or from the superior splenic
polar; or (3) a slender, thread-like cardioesophageal branch from the celiac
artery, aorta, first part of the splenic artery, or
inferior phrenic artery.
The terminal branches of the left
gastric anastomose with (1) branches of the right gastric; (2) short gastric
arteries from the splenic terminals or splenic superior polar or left
gastroomental; (3) cardioesophageal branches from the left inferior phrenic
(via its recurrent branch), an aberrant left hepatic artery from the left
gastric (A), or an accessory left gastric from the left hepatic (B) and from
descending rami of thoracic esophageal branches. The degree of anastomosis
about the cardioesophageal end of the stomach is variable; it may be very
extensive or very sparse.
In about one fourth of the
population, the left gastric artery gives off a large left hepatic artery (2 to
5 mm wide, 5 cm long) to the left lobe of the liver. Such a left hepatic may be
either replaced or accessory. In the replaced type (12%), no celiac left
hepatic is present, the entire blood supply to the lateral segment of the left
lobe being derived from the left gastric artery. The accessory
left hepatic is an additive vessel that supplies a region of the left lobe of
the liver (either the superior or inferior area of the lateral segment) not
supplied by the incomplete celiac left hepatic. From the functional point of
view, none of the hepatic arteries is ever “accessory” because every hepatic
artery supplies a definite region of the liver. In view of prevalent anatomic
variations, every gastric resection should be preceded by an exploratory examination
to determine what type of left gastric artery is present, for severance of a
left hepatic derived from the left gastric results in ischemia and fatal
necrosis (7th to 16th day) of the left lobe of the liver, as repeatedly
evidenced in postmortem examinations. Quite frequently, the left gastric gives
off an accessory left inferior phrenic and, in some instances, the left
inferior phrenic itself.
The celiac trunk may be incomplete
when the right or left hepatic arteries arise from some other source. The
common hepatic artery may arise in its entirety from the superior mesenteric
artery (C); the superior mesenteric artery may provide the right hepatic artery
in its entirety, also supplying blood to the gallbladder (D); and the superior
mesenteric artery may supply an accessory right hepatic artery, which may or
may not supply the gallbladder (E). The common hepatic artery may also branch
very proximally, giving off an early right and left hepatic arteries while the
right hepatic and gastroduodenal arteries branch from each other further to the
right (F). The left lobe of the liver may also receive an accessory left
hepatic artery from the right hepatic artery (G), or the right hepatic artery
may cross anterior to the hepatic duct before entering the substance of the
liver (H).
 |
| ARTERIES OF STOMACH, DUODENUM, PANCREAS, AND SPLEEN |
Invariably, the right gastric
artery is much smaller (2 mm) than the left gastric (4 to 5 mm), with which it
anastomoses. On occasion (8%) it gives off the supraduodenal or a spray of
twigs to the first part of the duodenum. Predominantly, the gastroduodenal
artery arises from the common hepatic (75%), but, in some instances, especially
with a split celiac trunk, it may arise from the left hepatic (10%), right
hepatic (7%), replaced hepatic trunk from the superior mesenteric or aorta (3.5%),
or even directly from the celiac or superior mesenteric artery (2.5%). These
atypical origins are correlated with the mode of branching of the celiac
artery, for the common hepatic may divide only into the gastroduodenal and
right hepatic (leaving the left hepatic to be replaced from the left gastric)
or into the gastroduodenal and left hepatic with replacement of the right
hepatic from the superior mesenteric. Typical branches of the gastroduodenal
are (1) the posterior superior pancreaticoduodenal (90%); (2) the anterior
superior pancreaticoduodenal; and (3) the right gastroomental. Inconstant
branches are (1) the right gastric (8%); (2) the supraduodenal (25%); (3) the
transverse pancreatic (10%); (4) a cystic artery, either the superficial branch
or the entire cystic (3%); (5) an accessory right hepatic; and (6) the middle
colic or an accessory middle colic (rarely).
The relatively large posterior
superior pancreaticoduodenal artery (1 to 3 mm in width) forms an arcade on the
back of the head of the pancreas, with branches to the duodenum. In many
instances (10%), the artery arises from a source other than the
gastroduodenal and, when it arises from the latter, it does so as its uppermost
collateral branch and not as an end branch. The right gastroomental artery is
considerably larger than the left gastroomental and, in its course, extends far
beyond the midline of the greater curvature of the stomach, where it
anastomoses with the left gastroomental artery. Of great surgical import is the
fact that, in many instances (10%), this anastomosis is not grossly visible, it
being absent or reduced to small arterial twigs that dwindle to
nothing before the two meet. The infragastric omental arc, formed by the right
and left gastroomental arteries, gives off a large pyloric branch and then a
variable number of ascending gastric and descending omental or anterior omental
branches. The omental branches descend between the two anterior layers of the
great omentum. The short ones anastomose with neighboring vessels, and the long
ones proceed to the distal free edge of the great omentum, where they turn
upward to become the posterior omental arteries. Many of
these join the large omental arc situated in the posterior layer of the great
omentum below the transverse colon. The arc is usually formed by the right
omental (first branch of the right gastroomental) and left omental, a branch of
the left gastroomental. Slender arteries ascend from the arc and anastomose
with similar branches (posterior omentals) given off from the middle colic or
left colic and from the transverse pancreatic coursing along the inferior
surface of the pancreas. The ultimate and penultimate branches of the posterior
omental arteries anastomose with the vasa recta of the middle colic but, apparently,
are not of sufficient caliber to take over the blood supply if the middle colic
has been rendered functionless. Aberra- tions of the right gastroomental are
(1) an origin from the superior mesenteric (1.5%) or with the middle colic and
superior pancreaticoduodenal (1%); (2) anastomoses with the middle colic, via a
large vessel (1%); and (3) an origin from a gastroduodenal derived
from the superior mesenteric.
Usually, the left gastroomental
arises from the distal end of the splenic artery (75%) or from one of its
splenic branches (25%) near its terminus. It may be replaced by two to three
vessels, the main artery coming from the splenic trunk and the others from an
inferior splenic polar artery. Branches of the left gastroomental are (1) short
fundic branches (two to four); (2) a variable number of ascending short gastric
arteries; (3) several short and long descending omental branches, some of which
communicate with similar branches from the right gastroomental artery; (4)
pancreatic rami to the tail of the pancreas, one of which, when large, is
termed the artery to the tail of the pancreas; (5) an inferior splenic polar
artery; and (6) the left omental artery, which descends in the great omentum to
form the left limb of the omental arc, the right limb being formed by the right
omental artery from the right gastroomental or transverse pancreatic artery.
 |
| ARTERIES OF DUODENUM AND HEAD OF PANCREAS |
The blood supply of the duodenum
and head of the pancreas is one of the most variant in the body and, surgically
considered, one of the most difficult to manipulate. The first inch of the
duodenum is a critical transition zone. Paucity or insufficiency of its blood
supply has repeatedly been correlated causatively with the tendency of ulcers
to perforate the superior part of the duodenum just beyond the pylorus.
Typically, the superior, anterior, and posterior surfaces of the first inch of
the duodenum are supplied by the supraduodenal artery, which may be derived
from either of two nearby arteries, the posterior superior pancreaticoduodenal
artery or gastroduodenal and, in the remaining cases, from the right gastric,
hepatic, or right hepatic. The supraduodenal artery frequently communicates
with branches of the right gastric, gastroduodenal, and anterior and posterior
superior pancreaticoduodenal arteries. The remaining portions of the duodenum
are supplied by branches from two pancreaticoduodenal arcades, one anterior and
the other posterior to the head of the pancreas. It is by virtue of these two
arcades that the duodenum is the only section of the gut that has a double
blood supply, one to its anterior surface and one to its posterior surface.
The anterior pancreaticoduodenal
arcade is formed by the anterior superior pancreaticoduodenal artery, the
smaller of the two end branches of the gastroduodenal artery. After making a
loop of a half circle or less on the anterior surface of the pancreas, medial to the
groove between the pancreas and duodenum, it sinks into the pancreas, turns to
the left, and ascends, and upon reaching the posterior surface of the head of
the pancreas, joins the anterior inferior pancreaticoduodenal artery, a
branch from the superior mesenteric artery. The arcade gives off 8 to 10
relatively large branches to the anterior surface of all three portions of the
duodenum and, in many instances, 1 to 3 branches to the first part of the
jejunum; they reach the jejunum by passing deep to the superior
mesenteric artery. The arc also supplies numerous pancreatic branches, some of
which are arranged in arcade fashion and anastomose with branches given off by
the dorsal pancreatic artery, derived from the first part of the splenic or
hepatic artery.
The posterior
pancreaticoduodenal arcade is made by the posterior superior
pancreaticoduodenal artery, which is the first branch of the gastroduodenal
given off by the latter above the duodenum above the upper border of the
head of the pancreas, where it may be hidden by connective tissue. In about 10%
of cases, it has a decidedly different origin, being derived from the hepatic
(4%), right hepatic (2%), aberrant right hepatic from the superior mesenteric
(3%), or dorsal pancreatic (1%). After its typical origin from the
gastroduodenal, the artery (1 to 3 mm in width) descends for 1 cm or more on
the left side of the common bile duct and then, after crossing the latter
anteriorly, descends for several centimeters along its right side before
swinging to the left and downward to form the posterior arcade. The major
portion of the U- or V-shaped posterior arcade lies posterior to the head of the
pancreas, at a level superior to that of the anterior arcade. It comes into
full view when the duodenum is mobilized and turned forward to expose its
posterior surface. It is covered by a fold of connective tissue sufficiently
thin that its branches can be seen. It is accompanied by a venous arcade that
lies superficial to the arterial arcade and that empties directly into the
portal vein. The arcade crosses the intrapancreatic part of the common bile
duct (to which it supplies blood) posteriorly. Ultimately, the posterior
superior pancreaticoduodenal artery unites with the inferior
pancreaticoduodenal artery derived from the superior mesenteric at a higher
level than that of the anterior arcade (40%), or it anastomoses with a
posterior branch of a common inferior pancreaticoduodenal, the latter receiving
both the anterior and posterior arcades (60%). The main branches, arising from
the posterior pancreaticoduodenal arcade, are (1) several descending branches
(two to three) to the first part of the duodenum, one of which may be the
supra- duodenal; (2) duodenal branches to the posterior surfaces of the
descending, transverse, and ascending duodenum; (3) small pancreatic branches
that are far less numerous and are shorter than those of the anterior arcade; (4)
ascending branches (one or more) to the supraduodenal portion of the common
bile duct; and (5) a cystic artery (entire or its superficial
branch), which, in about 4% of cases, stems from the first part of the
posterior superior pancreaticoduodenal or at its site of origin from the
gastroduodenal. In the majority of instances, the anterior and
posterior pancreaticoduodenal arcades have a variant anatomic structure, in the
sense that the arcades may be double, triple, or even quadruple. When multiple
arcades are present, it is the outer arcade near the duodenum that usually
supplies the latter with its branches, whereas the inner arcades supply only
pancreatic branches and ultimately become united with other branches of the
celiac trunk.
 |
| HEPATIC ARTERY VARIATIONS |
With every duodenal resection,
three important vascular arrangements must be borne in mind:
1. The entire
blood supply of the duodenum and head of the pancreas may be completely
dissociated from the superior mesenteric. This occurs when an aberrant right
hepatic from the superior mesenteric, coursing behind the head of the pancreas,
gives off one or two inferior pancreaticoduodenal arteries to receive the
anterior or posterior pancreaticoduodenal arcade (or both).
2. The
anterior or posterior pancreaticoduodenal arcade (or both) often ends via one
or more inferior pancreaticoduodenal arteries derived
from the left side of the superior mesenteric or from its first, second, or
third jejunal branch, a fact to be explored in every gastrojejunostomy, lest
the blood supply of the duodenum be impaired and rendered insufficient for
viability of that section of the gut.
3. In
resections of the duodenum, extreme care should be taken to maintain an
adequate blood supply to the anterior and posterior surfaces
of the stumps. The duodenal branches from the pancreaticoduodenal arcades are
end arteries, and if these are ligated, the suture lines pass through ischemic
parts that may become necrotic and break. This can result in “blowout” of the
duodenal stump; such an event has repeatedly been fatal, excessive
devascularization of the stump being the direct cause of the fatal
issue.




