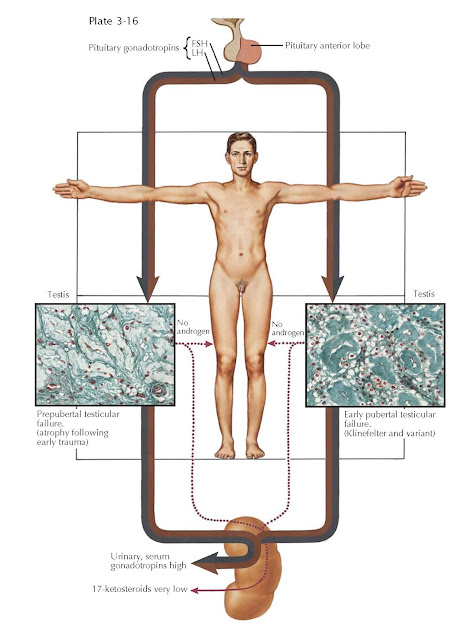
TESTIS FAILURE I: PRIMARY (HYPERGONADOTROPIC) HYPOGONADISM
Testicular failure may be unicompartmental and involve only exocrine function (spermatogenesis), or it may be bicompartmental and involve exocrine and endocrine (androgen) function. Endocrine deficiency due to interstitial or Leydig cell failure almost uniformly includes spermatogenic failure. Hypogonadism was originally used to delineate endocrine deficiency but customarily also refers to exocrine failure. Absence (e.g., castration, agenesis) of the testis is termed anorchia (formerly “eunuchism”). The term eunuchoidal habitus has been used to indicate a male body configuration that is characteristic of long-term androgenic deficiency, regardless of etiology.
Testicular deficiency is
classified clinically as (1) primary (or intrinsic) testicular failure beginning
prepubertally or very early in puberty, (2) primary testicular failure during
puberty (see Plate 3-16), (3) secondary testicular failure from pituitary
insufficiency or its variants (see Plates 3-17 and 3-18), and (4) predominantly
germ cell failure and infertility (see Plate 3-21) without androgenic failure.
Primary testicular failure
results from defects within the testis, usually occurring in the embryonic or
prepubertal periods. Pituitary function is unimpaired, because there exists a
compensatory rise in gonadotropin production during and after puberty. It is
also called hypergonadotropic hypogonadism. There is generally significant
testicular atrophy, characterized histologically by sclerosis of the infantile
(small) seminiferous tubules and a disappearance of Leydig cells in the
interstitium and replacement with hyalinization. Genetic causes of testis
atrophy include Klinefelter syndrome and its variants. Acquired causes are
mumps with orchitis, bilateral trauma, neonatal or postnatal torsion, or cryptorchidism.
Testis atrophy may also occur after chemotherapy or x-ray exposure from cancer
therapy and as a consequence of bilateral inguinal herniorrhaphy.
The physical habitus of an
affected male varies considerably, depending upon whether the testis failure
occurs before, during, or after puberty. Persistence of prepubertal physical
features after puberty with failure of pubertal progression occurs with testis
failure in childhood or during puberty. Patients may be tall and thin owing to
marked overgrowth of the long bones. Bone age and maturation may be greatly
delayed, and open epiphyses have been observed in affected
25-year-olds. Generally, the legs and forearms grow disproportionately long,
resulting in a greater distance from the symphysis to the heel than from the
symphysis to the top of the head. The arm span exceeds that of height by one or
more inches. Genu valgum and kyphosis in later life and significant osteoporosis
are also frequently encountered. The requirement for the development of eunuchoid
features is androgen deficiency during the period of rapid
growth at puberty, regardless of the reason. As such, these physical
characteristics are not restricted to patients with primary testicular failure
but are common to all types of testis failure. Indeed, castration or estrogen
administration after puberty during adult life does not cause regression of
male secondary sex characteristics and only minimally alters physical features,
except for gynecomastia, obesity, and skin changes.