PSORIASIS
Psoriasis is an autoimmune disease that affects 1% to 2% of the U.S. population. There is a large regional variation in the incidence of psoriasis. Scandinavian countries have a much higher incidence than the rest of the world, and the Native American population has one of the lowest rates of psoriasis. Much has been learned about the pathogenesis of psoriasis, and dramatic advances in therapy have helped many patients. Psoriasis is grouped with the other papulosquamous skin diseases. It can cause not only skin disease but also joint disease. The total effect that psoriasis has on patients cannot be judged solely on the basis of skin involvement, because the disease has been shown to have pro-found psychological and social effects as well. There is no known cure for psoriasis, but research is moving forward, and new therapies are being developed.
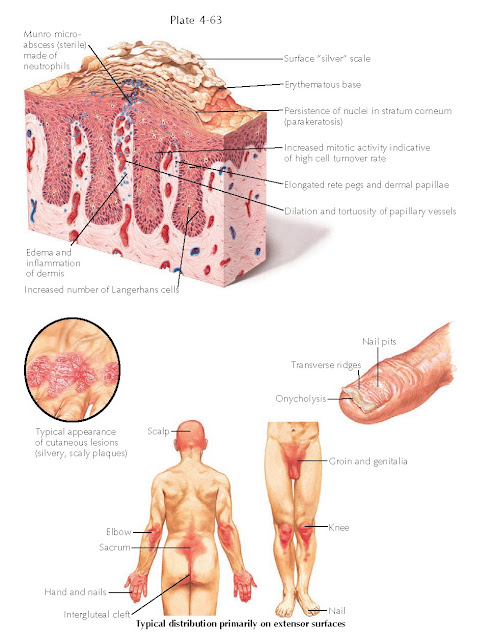 |
| HISTOPATHOLOGICAL FEATURES AND TYPICAL DISTRIBUTION OF PSORIASIS |
Clinical Findings: Psoriasis is a papulosquamous skin disease that can affect people at any
age of life. There is no gender predilection. Approximately 40% of affected
individuals have a family history of psoriasis. Most patients with early age at
onset tend to have a more severe course of disease. Psoriasis often starts with
silvery, ostraceous, scaly patches and plaques with a predilection for the
knees, elbows, and scalp. The term ostraceous scale refers to the oyster
shell–like appearance of the hyperkeratotic scale that is oriented in a concave
manner. The term rupioid scale is used to describe the psoriatic plaques
that appear to mimic the cone shape of limpet shells. A characteristic clinical
finding is that of Woronoff’s ring, the peripheral rim of blanching seen around
the early psoriatic plaques. Auspitz’s sign is another characteristic clinical
sign used to differentiate psoriasis from other rashes. It refers to the
pinpoint bleeding that occurs after the upper scale has been removed from a
psoriatic plaque. Woronoff’s sign is specific to psoriasis and most likely is
caused by localized vasoconstriction surrounding the area of the lesion, which
has an increased blood flow. There is a striking symmetry to the rash.
Psoriasis can have various skin morphologies. There are many well- recognized
clinical variants with distinctive clinical findings.
Psoriasis vulgaris is the most common form of
psoriasis encountered. It manifests with symmetrically located, silvery, scaly
patches and plaques on the scalp, knees, elbows, and lower back. Patients can
have a small amount of body surface area involvement, or they can have
widespread disease approaching near- erythroderma. The face is usually spared
from patches and plaques of psoriasis. Patients with a higher body surface area
of involvement tend to have a higher risk for development of psoriatic
arthritis and psoriatic nail disease. All patients with psoriasis exhibit the
Koebner phenomenon. Koebnerization of psoriasis occurs when a previously normal
area of skin is traumatized and psoriatic plaques develop within the
traumatized skin.
Inverse psoriasis is a well-recognized clinical
variant that manifests in intertriginous areas of the groin, gluteal cleft,
axillae, and umbilicus. The patches tend not to be as thick as in the other
forms, and the scale is fine. This is due to their location in occluded areas,
which have an increased amount of moisture and help to keep the scale to a
minimum. The patches can be bright red and are often misdiagnosed as a
cutaneous Candida infection. Inverse psoriasis is also symmetric in nature and can present
therapeutic challenges.
Guttate psoriasis is a variant of psoriasis that can
occur after an infection, most notably a streptococcal bacterial infection. The
guttate lesions develop soon after or during the infection and appear as tiny
teardrop-shaped patches with fine adherent scale. The word guttate means
“droplet,” and the lesions of guttate psoriasis appear as tiny droplets of psoriatic patches found generalized
over the skin, as if areas of psoriasis had developed within sprinkled water
droplets. Children with guttate psoriasis may have only one isolated episode
after a streptococcal infection and no evidence of psoriasis thereafter. Adults
with guttate psoriasis, on the other hand, almost always develop psoriasis
vulgaris at some later point.
Scalp psoriasis is a unique variant that occurs only
on the scalp. Patients complain of thick, scaly patches that itch and can cause
a dramatic amount of seborrhea. Most patients who present with localized scalp
psoriasis eventually develop areas of psoriasis elsewhere on their bodies.
Pustular psoriasis is a rare and distinctive form. It
can occur in patients with a preexisting history of psoriasis, or it can be the
initial presenting morphology. The diagnosis is straightforward in a patient
with a long- standing history of psoriasis who develops a pustular flare. The
most common reason for this is the rapid withdrawal of systemic
corticosteroids, for example, when a patient with psoriasis is prescribed
methyl- prednisolone for some unrelated condition, such as allergic contact
dermatitis due to poison ivy. The rapid decrease in the dose of the
corticosteroid can induce a pustular flare. The patches of psoriases develop
pin-point (1-2 mm) pustules that can coalesce into superficial pools of pus.
These patients are often ill appearing and can have associated hypocalcemia.
Patients presenting with pustular psoriasis without a preexisting history of
psoriasis pose a difficult diagnostic problem at first. The differential diagnosis
is among psoriasis, a pustular drug eruption, and Sneddon-Wilkinson disease. A
skin biopsy and clinical follow-up will eventually make the diagnosis clear.
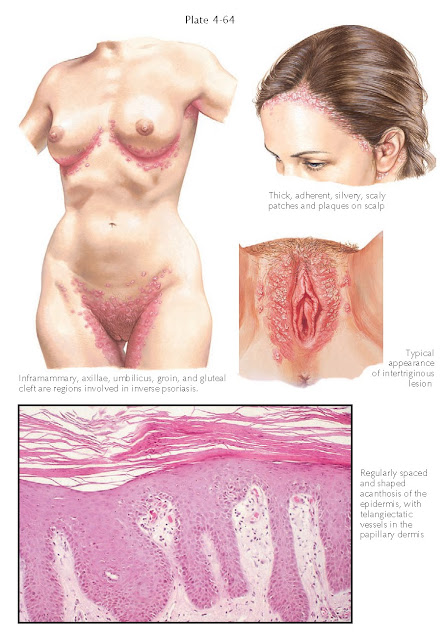 |
| INVERSE PSORIASIS AND PSORIASIS IN THE GENITAL AREA |
Nail psoriasis is most often associated with severe
psoriasis vulgaris and psoriatic arthritis. It can occasionally be a solitary
finding. Oil spots, onycholysis, nail pitting, and variable amounts of nail
thickening can be present. Nail disease is refractory to most topical
therapies, and often systemic therapy is required to get a good clinical response.
Nail psoriasis is a marker for psoriatic arthritis, and patients with nail
psoriasis are at a higher risk for development of psoriatic arthritis.
Palmar and plantar psoriasis is another of the less
commonly seen clinical variants. It can manifest on the palms and soles as red,
scaly patches and plaques or as patches studded with a variable amount of small
pustules. This variant of psoriasis is more commonly found in females, and
smoking has been shown to make the clinical course worse.
Psoriatic erythroderma is a rare variant that is seen
as a sequela of steroid withdrawal or of other, undefined triggers. It
manifests with near-total redness of the skin. The redness is caused by massive
vasodilatation of the cutaneous vasculature, which can lead to high-output
cardiac failure. These patients are universally treated in the inpatient
setting.
Psoriatic arthritis can manifest in association with
psoriatic skin disease or as arthritis with nail findings. Patients typically present with an asymmetric oligoarticular
arthritis, a symmetric polyarticular arthritis, distal
interphalangeal–predominant disease, spinal spondylitis, or arthritis mutilans.
Arthritis mutilans is the rarest form of psoriatic arthritis, but it is life
altering and can lead to a devastating loss of function. Psoriatic arthritis is
considered to be a seronegative form of inflammatory arthritis.
Pathogenesis: Psoriasis is
an autoimmune disease caused by an abnormality within the cells of the immune
system. There is a genetic susceptibility, and the human leukocyte antigen
(HLA) Cw6 locus is the most commonly found (but not the only) susceptibility
factor in patients who develop psoriasis. The success of therapy with
cyclosporine, a medication that dramatically decreases T-cell function, was one
of the first clues to the
pathogenesis of psoriasis. Psoriatic patients given this medicine almost always
have rapid clinical improvement.
T-cell lymphocytes and dermal dendritic cells are the
most likely precursor cells to be the cause of psoriasis; they are both found
in increased numbers in psoriatic plaques. CD8+ T cells are the predominant
lymphocyte found within the epidermis; they contain the cutaneous lymphocyte
antigen (CLA) antigen on their cell surface. The CLA antigen is important
because it directs these cells into the skin. Many subsets of dermal dendritic
cells have been found within psoriatic plaques. Dendritic cells have been shown
to be potent stimulators of T cells, and they are believed to be required to
propagate the inflammatory reaction. These two cell types interact with each
other and change the local cytokine profile into one that is proinflammatory
and provides a milieu that is required for the development of the clinical
findings of psoriasis. What is still unknown is the initial stimulus that sets
off this cascade of events and how it is propagated and perpetuated.
 |
| PSORIATIC ARTHRITIS |
Histology: Histological
examination of biopsy specimens of psoriasis vulgaris show regular psoriasiform
hyperplasia of the epidermis. Multiple normal-appearing mitotic figures are
seen within keratinocytes. Neutrophils are prominent within the stratum corneum
and within the lumen of the papillary dermal blood vessels. Mounds of
parakeratosis are seen in the stratum corneum and contain many neutrophils. The
papillary dermis shows a proliferation of ectatic capillary vessels with a
perivascular infiltrate made up of lymphocytes, Langerhans cells, and histiocytes.
Collections of neutrophils within the stratum corneum are called Munro
microabscesses. Kogoj microabscesses are similar collections of neutrophils
within the stratum spinosum. There is a decrease in the thickness of the
granular cell layer. With time, some of the tips of the rete ridges coalesce
and form thickened ends.
Pustular psoriasis shows varying amounts of
intraepidermal pustules; acanthosis and psoriasiform hyperplasia are not
prominent. Again, there are multiple dilated capillary blood vessels in the
papillary dermis.
Treatment: There is no
cure for psoriasis. Treatment should be based on the amount and location of the
psoriatic plaques and consideration of the psychological well-being of the
affected individual. Small areas in discrete locations can be treated with
topical corticosteroids, anthralin, tar compounds, or vitamin D or A analogues
or left alone without therapy. Ultraviolet therapy with natural sunlight,
narrow-band ultraviolet B light (UVB), or psoralen + ultraviolet A light (PUVA)
has been used with great success. Often, combinations of therapies are
implemented.
As the body surface area of involvement increases or
the psychological well-being of the individual is affected such that systemic
therapy is warranted, many agents are available to treat the psoriasis.
Phototherapy with narrow-band UVB or PUVA has been used for decades with excellent results. In the long term, these
therapies increase the patient’s risk of developing skin cancers, and lifelong
dermatologic follow-up is required.
Oral systemic agents are also used for moderate to
severe psoriasis. Methotrexate taken on a weekly basis has been used for years.
Oral cyclosporine has been used with great success for erythrodermic and
pustular psoriasis. Its use is limited to 6 to 12 months because of
nephrotoxicity. Many biological agents have become available over the last decade. These medications are
given by subcutaneous, intramuscular, or intravenous injection. They include
etanercept, alefacept, adalimumab, infliximab, and ustekinumab. All of these
agents have had excellent response rates. They are all considered to be
immunosuppressive, and patients taking these medications need close clinical
follow-up, because they are at increased risk for infections and possibly for
systemic cancers, such as lymphoma, after years of use.




