PSEUDOXANTHOMA ELASTICUM
Pseudoxanthoma elasticum is a rare genetic disorder with both cutaneous and systemic findings. It is inherited in an autosomal recessive manner. This disease is caused by a defect in an adenosine triphosphate (ATP) binding protein that is found in many tissues, including the skin, eye, gastrointestinal tract, and cardiovascular systems. The cutaneous findings often precede the appearance of the systemic findings. Recognition of the cutaneous findings can help lessen the risk of systemic complications. A multidisciplinary approach to the care of these patients is required. The skin findings have no bearing on mortality.
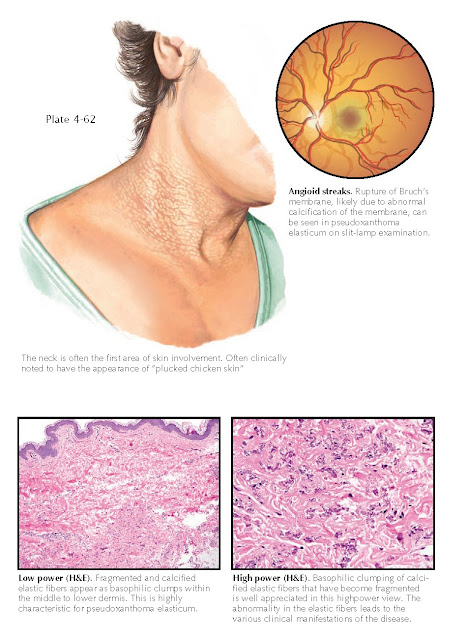
Clinical Findings: Pseudoxanthoma elasticum manifests in late childhood or early adulthood.
The cutaneous findings are almost always the first sign of the disease. The
skin on the neck is most commonly affected early and most severely. There is a
“plucked chicken” appearance to the skin. Small yellow papules are studded
within the involved region, and over time they coalesce into larger, symmetric
plaques. The intervening skin has a dull appearance with a fine pebbly texture.
The neck is by far the area most noticeably affected, but other regions may
become involved, including the intertriginous regions. A rare generalized
cutaneous form has been reported. The mucous mem- branes may also become
involved with tiny yellow papules. As time progresses, the skin may become
loose, appearing to hang from the body, and this can be a significant cosmetic
concern to the patient. The areas of cutaneous involvement are essentially
asymptomatic. On occasion, mild pruritus is reported. A nonspecific skin
finding that is seen with increased frequency in pseudoxanthoma elasticum is
elastosis perforans serpiginosa. This perforating disorder has been described
to occur in many different clinical settings, and it is caused by the
transepidermal elimination of damaged elastic tissue. The reason this occurs in
pseudoxanthoma elasticum is unknown.
It is important to diagnosis this disease at a young age so that some of the severe systemic complications
can be prevented. The globe is affected in pseudoxanthoma elasticum. The first
sign is a yellowish discoloration of the retina. Later in life, cracks or
ruptures in Bruch’s membrane can be seen on funduscopic examination; these are
termed angioid streaks. Angioid streaks have a later age at onset than
the cutaneous findings do. Abnormalities of the elastic fibers in Bruch’s
membrane are responsible for their formation. Angioid streaks can be seen in
many disorders of connective tissue and are not specific for pseudoxanthoma
elasticum. Retinal hemorrhage and resultant visual field loss is the most
severe ophthalmological complication.
Cardiovascular and gastrointestinal manifestations
arise because of the abnormal calcification of elastic tissue within blood
vessel walls. Gastrointestinal hemorrhage may occur and may be
life-threatening. Angina and hypertension may occur from involvement of the
coronary and renal arteries, respectively.
Histology: Findings on
skin biopsies are very characteristic and show abnormal fractured, calcified
elastic tissue within the dermis. The findings can be accentuated with special
staining methods to highlight the calcified elastic fibers. However, the
diagnosis can be made easily on routine hematoxylin and eosin staining.
Pathogenesis: Pseudoxanthoma
elasticum is inherited in an autosomal recessive fashion and is caused by a
defect in the ABCC6 gene. This gene is responsible for encoding the
multidrug resistance associated protein 6 (MRP6), which is also known as ATP-binding cassette transporter 6
(ABCC6). This protein is found within the liver and kidneys and is expressed at
low levels in the tissues that are affected by this disease. It has been
proposed that the defect causes a metabolic abnormality, possibly resulting in
a buildup of a metabolite that damages to the elastic fibers in the affected
tissue.
Treatment: Therapy is
directed at preventive care. Routine cardiovascular and ophthalmological examinations can help keep hypertension and early
signs of retinal disease in check. Retinal hemorrhages need to be treated
acutely by an ophthalmologist. Routine examinations for blood in the stool and
routine gastrointestinal examinations are warranted to screen for gastro-
intestinal bleeding, which is the main cause of morbidity and mortality in
these patients. Patients should be encouraged to stay within a healthy weight
range and not to smoke. Most
patients live a normal life span.