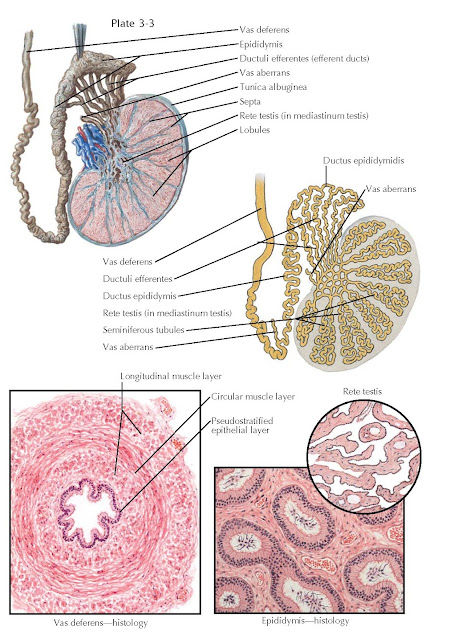
TESTIS, EPIDIDYMIS, AND VAS
DEFERENS
The testicle is encased within a thick, fibrous capsule known as the
tunica albuginea. The tunica is covered by the closely adherent, glistening
peritoneum (tunica vaginalis). Multiple septa from the capsule divide the
interior of the testicle into several dozen pyramid- shaped lobules. The testis
shows ethnic variations in size, but is normally 4 cm in length and 3 cm in
diameter (18 to 20 mL in volume).
Within each testicle, each
lobule contains one or several tortuous seminiferous tubules which, when
uncoiled, measure 1 to 2 ft in length. These tubules converge at the testicular
hilum (mediastinum testis), where they straighten and anastomose to form the
rete testis. The rete testis tubules empty into 8 to 10 efferent ducts (ductuli
efferentes) that carry sperm to the caput epididymis. Occasionally a
blind-ending efferent duct is observed (vas aberrans). Spermatoceles are
thought to be the result of pathologic dilation of the efferent ducts.
Testicular histology reveals
evidence of both exocrine (sperm production) and endocrine (androgen
production) functions within the organ. In the normal, adult testis,
seminiferous tubules are lined with a basement layer of laminated connective
tissue containing elastic fibers and flattened myoid cells. On this layer rests
the germinal epithelium and sustentacular cells known as Sertoli cells. The
intertubular connective tissue contains groups of large polygonal cells termed
Leydig cells, whose cytoplasm holds many lipid granules that contain
testosterone and other androgens. Characteristics of maleness, including body
hair, muscle mass, deepened voice, and sexual function are several androgen dependent functions.
The epididymis is a
comma-shaped organ located along the posterolateral surface of the testis. It
is a tightly coiled, tortuous duct 3 to 4 m in length, embedded in dense
connective tissue. Passage through the epididymis induces many changes to newly
formed sperm, including a gain in functional motility and alterations in
surface charge, membrane proteins, immunoreactivity, phospholipids, fatty acid
content, and adenylate cyclase activity. These changes improve cell membrane
structural integrity, increase fertilization ability, and improve motility.
Spermatozoa within the testis have very poor or no motility. They become
progressively motile and functional only after traversing the epididymis. The
transit time of sperm through the epididymis has been estimated at 12 days in
humans.
Extensions from the tunical
sheath that surrounds the epididymis enter interductal spaces and form septa
that divide the duct into histologically characteristic regions: the caput or
head, corpus or body, and cauda or tail. The 8 to 10 ductuli efferentes within
the caput region coalesce to form a single epididymal duct within the corpus
and cauda epididymis. The epididymis is distinguished histologically by its
ciliated epithelium that consists of two main cell types: principal cells and
basal cells. Principal cells vary in height along the length of the epididymis
mainly because of the length of associated stereocilia. Principal cell nuclei
are elongated and often possess large clefts and one or two nucleoli.
Consistent with absorptive and secretory function, their cellular apices have
numerous coated pits. There are far fewer basal cells than principal cells in
the epididymis. Tear-shaped basal cells rest on the basal lamina and extend
approximately toward the lumen, their apices forming threads between adjacent
principal cells. Thought to be derived from macrophages, they
are likely the precursors of the principal cells.
The vas deferens originates
as a continuation of the cauda epididymal duct. During this transition, the
muscular coat of the tubule increases dramatically, the tortuosity of the duct
decreases, and epithelial cells lose cilia. The vas continues for about 25 cm
and becomes the ampulla of the vas before joining with the seminal vesicle and
forming the proximal ejaculatory duct. In cross section, the vas deferens has
an outer adventitial
connective tissue sheath
containing blood vessels and small nerves, a muscular coat that consists of a
middle circular layer surrounded by inner and outer longitudinal muscle layers,
and an inner mucosal layer with a pseudostratified epithelial lining. The outer
diameter of the vas deferens varies from 1.5 to 3 mm, and the lumen of the
unobstructed vas deferens varies from 0.2 to 0.7 mm in
diameter, dimensions easily handled using microsurgical approaches to surgical
reconstruction after vasectomy or other blockage.