INJURIES TO THE FINGERTIP
As the sensory input to the upper extremities, the fingertips encounter
their environment first and are often unfortunately injured. Whether it be on a
sporting field or in the workplace the fingertips are subject to cuts, burns,
punctures, and sudden impact and crushing injuries. It is of paramount
importance to try and restore the fingertips for optimal hand and upper
extremity function.
Fracture Of The Distal Phalanx And Subungal Hematoma
Impact injury to the fingertip often causes a hematoma
due to bleeding from either the nail bed or an underlying fracture of the
distal phalanx. This hematoma is often trapped under the nail plate, causing
significant pressure to build up and resultant pain. When the pain is
significant, this can be relieved by drainage of the hematoma. It is important
to obtain a radiograph to rule out a fracture because, once drained, this hole
in the nail plate becomes a portal to an infection in the distal phalangeal
bone if not cared for appropriately. An old treatment of heating a paperclip
under a flame does not properly sterilize the metal tip, and therefore only a
sterile needle should be used. A 22-gauge needle can be used by hand to
adequately drill a small perforation in the nail plate and provide evacuation
of the hematoma. The patient should be given an antibiotic if the injury
dictates, and the nail plate should be kept clean. A short splint blocking the
distal interphalangeal joint will allow for pain relief and protection of the
underlying injured fingertip.
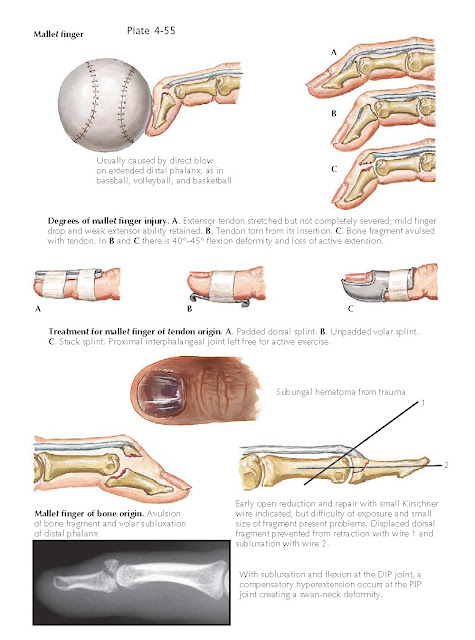
Mallet Finger
Hyperflexion that disrupts the extensor mechanism of
the distal phalanx causes a mallet finger, an injury common in ball players. Three types of injury occur:
stretching of the extensor tendon past its elastic limit, which causes multiple
interstitial tears; complete disruption of the extensor tendon; and avulsion
fracture of the base of the distal phalanx. The patient with mallet finger
often does not appreciate the severity of the injury, and even the examining
physician may not recognize the injury. The acute signs are tenderness over the
dorsum of the distal interphalangeal joint and inability to actively extend the
distal phalanx.
Treatment consists of splinting the distal
interpha-langeal joint in extension. The splint should be placed on the dorsal aspect during the day so the volar
surface of the finger can still be used in opposition; it is worn continuously
for 6 to 8 weeks, then only at night for an additional 3 to 4 weeks. A palmar
splint is used at night to relieve the continuous pressure on the dorsal skin.
The patient should be warned that splinting may cause some skin loss over the
dorsum of the distal phalanx and that full extension may never be regained.
Mallet finger with avulsion of a large bone fragment
may be associated with volar subluxation of the distal interphalangeal joint. Surgical repair, although
indicated, is difficult because the blood supply to the skin is poor, the
fragment is quite small, and a good reduction with Kirschner wires is often
difficult to maintain. Therefore, a dorsal blocking pin is more effective to
prevent proximal retraction of the tendon-bone complex. A pin across the joint
ensures concentric reduction and go d soft tissue healing to avoid recurrent
subluxation.