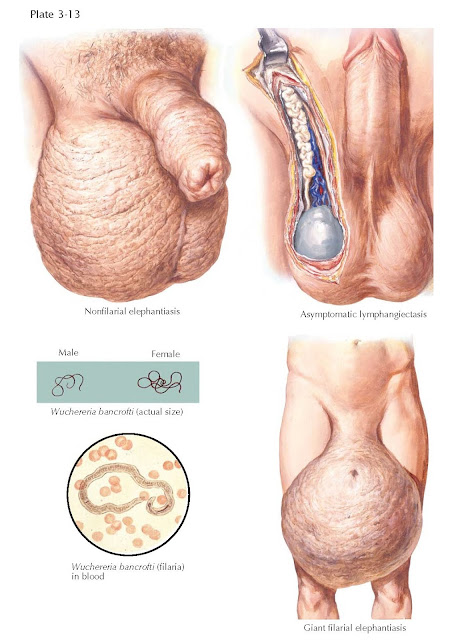
ELEPHANTIASIS
Filarial elephantiasis of
the scrotum presents as diffuse scrotal enlargement from hypertrophy and
hyperplasia of the subcutaneous tissues and epidermis, which become leathery,
coarse, and dry. Sebaceous glands are usually destroyed. The consistency of the
leathery skin is that of nonpitting edema. The scrotum varies in size from
slight enlargement to becoming monstrous in size, with the scrotum touching the
ground and weighing as much as 200 pounds. The condition is indigenous to
tropical areas. Filarial elephantiasis is caused by a nematode, Wuchereria
bancrofti (90%), and is transmit- ted to man by certain mosquito species (Culex,
Aedes, and Anopheles). Other thread-like parasitic worms such as Brugia
malayi (10%) and Brugia timori (1%) may also cause elephantiasis.
The adult worms in man are found in lymphatic channels and in subcutaneous
tissues; the larval forms usually enter the bloodstream between the hours of
midnight and 2 am. These microfilariae produce no general symptoms except those
associated with obstruction of lymphatics. Scrotal elephantiasis is a late
sequela of filarial infection and results from lymphatic obstruction. Secondary
bacterial infections can accentuate the process. Usually, a history of repeated
episodes of lymphangitis and lymphadenitis associated with fever, malaise,
rash, and tender lymph nodes after inoculation is obtained. With each episode
of diffuse enlargement and swelling, the regression and healing is less
complete. Superficial lymphatics may become dilated, rupture, and exude lymph.
Filariasis may begin as an
insidious condition known as “lymph scrotum,” which is characterized by a mild
enlargement of the scrotum along with cutaneous lymphatic ectasia. Three other
presentations have been described with filariasis. The first is somewhat similar
to lymph scrotum but involves the spermatic cord, which feels like soft,
compressible vessels. In another presentation, the spermatic cord contains
thick, rubbery masses, which represent a late fibrous reaction following
lymphangitis. In this presentation, fibrous nodules, distinct from the vas
deferens, are palpated throughout the spermatic cord. The third type of
presentation, called “mumu,” was observed during World War II as acute swelling
and edema of the spermatic cord that gradually subsides after individuals leave
an endemic area. This may represent an allergic reaction that develops
following filarial inoculation.
Although positive skin tests
and DNA polymerase chain reactions (PCRs) can detect filarial DNA and indicate
disease, the definitive diagnosis is made by finding the microfilariae in the
peripheral blood at night after filtration through micropore membrane filters.
This can also quantify the load of microfilariae. However, once lymphedema
develops, the microfilariae are absent in peripheral blood. Specific drug therapy
involves diethylcarbamazine (microfilaria and adult worms), ivermectin (microfilaria), albendazole (adult filarial worms), and
possibly even doxycycline. Once lymphedema develops, there is no cure but
reducing inflammation, and surgical removal of the elephantiasic genital tissue
may help in selected cases.
Alternatively, elephantiasis
may occur in the absence of parasitic infection. This nonparasitic form of
elephantiasis is known as nonfilarial elephantiasis or “podoconiosis,” and
occurs in high frequency in northern Africa. Nonfilarial elephantiasis is
thought to be caused by persistent contact with irritant
soils, or from lymphedema, lymph obstruction, or lymphangitis from a wide
variety of causes, including infection. This elephantiasis may occur as a
result of local disorders such as scrotal fistulae, or following inguinal
lymphadenectomy, metastatic carcinoma, or inguinal lymphangitis from syphilis,
lymphogranuloma venereum, tuberculosis, or granuloma inguinale. Treatment is
aimed at eradication of infection and
supportive care for the
enlarged scrotum.