Disorders Of The Adrenal Medulla
Phaeochromocytoma and paraganglioma
Definition
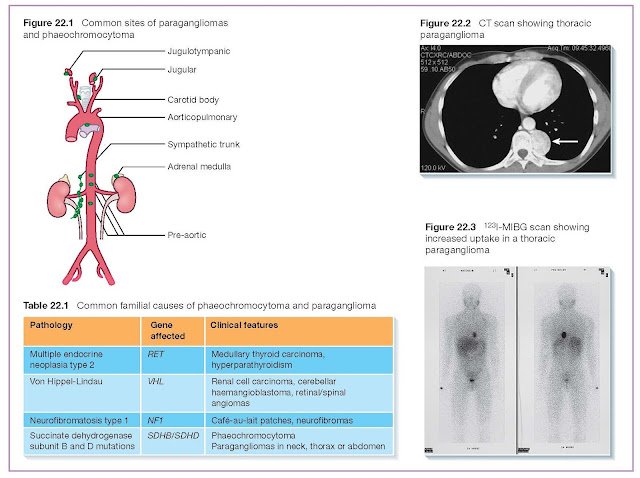
Phaeochromocytomas are catecholamine-secreting tumours which occur
in about 0.1% of patients with hypertension. In about 90% of cases they arise
from the adrenal medulla. The remaining 10%, which arise from extra-adrenal
chromaffin tissue, are termed paragangliomas (Figure 22.1).
Most phaeochromocytomas are sporadic but a genetic basis is
recognised in up to 30% of patients (Table 22.1), especially in bilateral,
extra-adrenal or malignant tumours (<10%).
Symptoms and signs
Common presenting symptoms include one or more of headache,
sweating, pallor and palpitations. Less commonly, patients describe anxiety,
panic attacks and pyrexia. Hypertension, whether sustained or episodic, is
present in at least 90% of patients. Left untreated, phaeochromocytomas can
occasionally lead to hypertensive crisis, encephalopathy, hyperglycaemia,
pulmonary oedema, cardiac arrhythmias or even death. Patients with undiagnosed
phaeochromocytomas having routine surgery can develop severe hypertension or
sudden death.
Investigations
Diagnosis relies on the biochemical confirmation of elevated
catecholamines or their metabolites (metanephrines), followed by radiological
localisation of the tumour.
Biochemistry
The biochemical screening investigation of choice is usually
24-hour urinary fractionated metanephrines with or without free catecholamines.
Two or more collections may be needed if the index of suspicion is high because
of the episodic nature of tumour secretion. Measurement of plasma metanephrines
has replaced urine collection in many centres, and is especially useful if
measured during symptoms or crisis. Serum chromogranin A levels, a marker of
neuro-endocrine hypersecretion, can be elevated in phaeochromocytoma or
paraganglioma.
Radiology
CT (Figure 22.2) or MRI of the abdomen are the initial imaging
modalities of choice, followed by whole-body MRI if the tumour is not
localised. 123I-meta-iodobenzylguanidine (MIBG) can locate tumours not seen on
MRI and is useful pre-operatively to exclude multiple tumours (Figure 22.3).
Genetic testing
Genetic testing is indicated in patients with syndromic
presentations but also in many apparently sporadic tumours, because up to 30%
harbour germline mutations in susceptibility genes. Mutations are more likely
in patients presenting at a young age, or in those with multifocal, malignant
or extra-adrenal disease. Identification of a predisposing mutation should lead
to annual screening for new or recurrent disease in index cases, and cascade
genetic testing of first degree relatives.
Management
The definitive treatment is surgical excision, which is performed
laparoscopically or through an open procedure. In advance of surgery, it is
mandatory that all patients are protected from the effects of catecholamine
excess by pharmacological alpha with or without beta-blockade. Alpha-blockade,
conventionally administered as oral phenoxybenzamine, should be commenced
before beta-blockade in order to avoid unopposed alpha-adrenergic stimulation
and the risk of hypertensive crisis. Beta-blockers can be introduced
subsequently to control reflex tachycardia.
Prognosis
Five-year survival for apparently benign tumours is 96% and the
recurrence rate is less than 10%. Successful surgical removal leads to cure of
hypertension in most patients. Malignant disease can be treated with 131-I MIBG
therapy or chemotherapy. There is increasing interest in the use of newer
radionuclides in both the diagnosis and treatment of metastatic disease.