DEFORMITIES OF INTERPHALANGEAL
JOINT
The collateral ligament system and the flexor and extensor tendons play
an important role in maintaining the normal configuration of the proximal
interphalangeal joint. The distal interphalangeal joint acts as a simple hinge
but is very important for balancing the proximal interphalangeal joint, and
hyperextension or flexion (mallet) deformity can cause boutonnière or swan-neck
deformities, respectively. The rheumatoid process compromises the normal
anatomy of the joint and may lead to joint stiffness, with or without lateral
deviation, or to collapse deformities, most notably boutonnière and swan-neck
deformities. Mallet finger is not common in rheumatoid arthritis but is common
in osteoarthritis. Limited joint movement may result from articular factors
(adhesions and disorganization of the joint), periarticular factors (adhesions
or laxity of ligaments), or tendinous factors (synovial invasion of the flexor
tendons and adhesions).
Collapse deformities of the three-joint system of the digit
are characterized by hyperextension of one joint and reciprocal flexion of
adjacent joints. The deformity occurs when the balance between the tendon and
ligament systems is compromised. Axially applied forces further aggravate the
deformity, establishing a cycle of deforming forces.
Boutonnière Deformity
This condition is characterized by flexion of the
proximal interphalangeal joint and hyperextension of the distal interphalangeal
joint (see Plate 4-31). In rheumatoid arthritis, causes of boutonnière
deformity include (1) capsular distention
of the proximal interphalangeal joint; (2) lengthening of the central long extensor
tendon, with lack of extension in the middle phalanx; (3) lengthening of the transverse fibers; (4) palmar
subluxation of the lateral bands, which become flexors of the proximal interphalangeal
joint; (5) increased extensor pull on the distal phalanx; (6) self-perpetuating collapse
deformity; and (7) soft tissue contracture, joint stiffness, and
disorganization.
Swan-Neck Deformity
The term swan-neck deformity refers to hyperextension
of the proximal interphalangeal joint and flexion of the distal interphalangeal joint (see Plate 4-31). In
rheumatoid arthritis, the deformity may result from (1) synovitis of the flexor
tendon sheath, which causes difficulty in initiating or completing flexion of
the interphalangeal joint; (2) increased flexor pull at the metacarpophalangeal
joint; (3) increased pull of the intrinsic muscles to the central tendon; (4)
loosened attachments of the palmar ligament and accessory collateral ligaments
of the proximal interphalangeal joint; (5) hyperextension of the proximal
interphalangeal joint; (6) stretching of the oblique retinacular ligaments; (7)
dorsal subluxation of the lateral bands, which become extensors of the proximal
interphalangeal joint; (8) pull of the flexor digitorum profundus tendon, which
flexes the distal interphalangeal joint; and (9) joint disorganization and
subluxation. Other factors that increase the mechanical advantage of the
extensor pull and accentuate the deformity include palmar subluxation of the
metacarpophalangeal or wrist joint and contracture of the intrinsic muscles secondary to chronic flexion deformity of the
metacarpophalangeal joint. In osteoarthritis, deformity typically starts with a
stiff flexion deformity of the distal interphalangeal joint.
Deformities Of Distal Interphalangeal Joint
In osteoarthritis and rheumatoid arthritis,
deformities of the distal interphalangeal joint are usually secondary to
collapse deformities. Specific deformities resulting from synovial invasion are
uncommon; however, loosening of the distal attachment of the extensor tendon
may cause a mallet or drop finger. Loosening of the collateral ligaments,
erosive changes in the subchondral bone, and cartilage destruction in combination
with external forces applied during daily activities may lead to joint
instability. Complete joint destruction may also occur secondary to the severe
resorptive changes seen in arthritis mutilans.
Surgery For Proximal Interphalangeal Joint
In swan-neck deformity, flexor synovitis is treated
first. If the articular surfaces are preserved, hemitenodesis of the flexor digitorum superficialis tendon to the base
of the middle phalanx can be done at the same time to check the hyperextension
deformity of the proximal interphalangeal joint. Usually, it is not necessary
to lengthen the central slip in release of the swan-neck deformity. It is
important to obtain adequate release of the dorsal capsule, collateral
ligaments, and palmar plate. A 10-degree flexion contracture (or greater) of the proximal
interphalangeal joint should be obtained and associated deformities of the
contiguous joints corrected.
In a mild flexible deformity in weak hands, dermadesis
is indicated: an elliptic wedge of skin (sufficient to create a 20-degree
flexion contracture) is removed from the flexor aspect of the proximal interphalangeal joint, preserving the
underlying vessels and nerves. If the articular surfaces are inadequate,
however, fusion of the proximal interphalangeal joint is preferred. Implant
arthroplasty is rarely indicated.
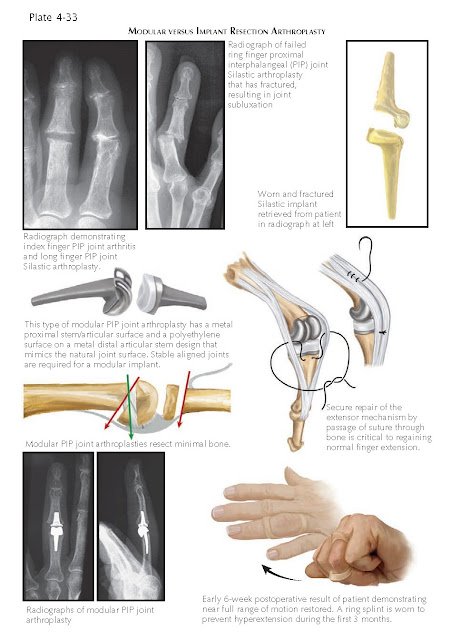
Treatment of arthritic deformities of this joint
includes realignment of the longitudinal arch of the digit. The joint can be
treated by arthrodesis, resurfacing arthroplasty, or resection implant arthroplasty.
Resurfacing of the proximal interphalangeal joint is indicated for painful,
degenerative, or posttraumatic deformities with destruction. When subluxation
of the joint that cannot be corrected with soft tissue reconstruction alone or
significant bone loss exists, implant resection arthroplasty is indicated. For
deformities of the proximal interphalangeal joints of both the index and long
fingers with osteoarthritis or early rheumatoid arthritis in a young person who
performs heavy labor, the proximal interphalangeal joint of the index finger is
fused in 20 to 40 degrees of flexion, and resurfacing or resection implant
arthroplasty is performed for the proximal interphalangeal joint of the middle
finger. The more stable index finger can be used in pinch, and the more
flexible long finger can be used in grasp. Flexion of the proximal
interphalangeal joints in the ring and little fingers is very important for
grasping small objects, and function should be restored if possible.
Good results require adequate release of joint contractures.
The collateral ligaments are left intact when-ever possible and if released
they should be released on both sides to prevent pivoting instability on the
intact side. Rebalancing and postoperative capsuloligamentous healing will
stabilize the joint when the postoperative protocol below is utilized. If the
joint is severely contracted, more bone is removed, or if too great and the
joint cannot reduced, an implant resection arthroplasty is used, allowing for even more bone resection. If the
contracture persists, the palmar plate and collateral ligaments may be incised
proximally or distally, as needed. The collateral ligaments are not required to
be repaired. Resurfacing arthroplasty may be placed either press-fit because they
have a bone ingrowth surface or cemented if a tight fit cannot be achieved.
Importantly, the central tendon is advanced slightly distal on the middle phalanx, which ensures
full extension postoperatively. A coexisting mallet deformity of the distal
interproximal joint must be corrected at the time of surgery to prevent a
swan-neck deformity.
The hand is dressed as in metacarpophalangeal joint
surgery, and 2 or 3 days after surgery, hand-based thermoplastic splints are applied with the finger in 0 degrees of
flexion for 3 to 4 weeks. Motion is initiated under supervision, and flexion is
gradually increased after 3 weeks as long as full extension can be obtained.
The resting splint can be applied slightly to the radial or ulnar side of the
digit to correct any residual tendency to deviate; it is worn at night and
between exercise periods until adequate healing occurs.
In an alternative approach, the central tendon is pre-
served and the exposure is volar, releasing the cruciate pulley, displacing the
flexor tendons, releasing the volar plate, and preserving the extensor tendon
insertion. Postoperative motion is immediate and preferred for resection
implant arthroplasty. However, visualization and correction of soft tissue and
bony deformity for resurfacing arthroplasty is more difficult to achieve and
may be incomplete.
Implant resection arthroplasty for proximal interphalangeal
joints with collapse deformity requires adjustment of the tension of the
central tendon and lateral bands as mentioned earlier. Compared with the
lateral bands, the central tendon is relatively tight in the swan-neck
deformity and must be released, while in the boutonnière deformity, the central
tendon is relatively loose and must be tightened.
Implant resection arthroplasty for boutonnière
deformity is accompanied by reconstruction of the extensor tendon mechanism.
The collateral ligaments are reefed or reattached to bone as needed. After
surgery, extension of the proximal interphalangeal joint and flexion of the
distal interphalangeal joint must be maintained. The proximal interphalangeal
joint is immobilized in extension with a padded aluminum splint for 3 to 6
weeks; the distal joint is allowed to flex freely. Active flexion and extension
exercises are started 3 to 4 weeks after surgery, and a splint should be worn
at night for about 10 weeks.
Surgery For Distal Interphalangeal Joint
If the distal interphalangeal joint is unstable,
subluxated, or deviated or if there is articular damage, arthrodesis is the
treatment of choice. Contractures of the joint may be treated with soft tissue
release and temporary fixation with a Kirschner wire to allow some useful residual movement.
Slight flexion movement of the distal interphalangeal joint is very important
in finely coordinated activities, but if movement at the proximal
interphalangeal joint is good, fixation in a functional position is acceptable.