CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Chronic obstructive
pulmonary disease (COPD) is a chronic disease that is defined by progressive
airflow obstruction that is not completely reversible. COPD is caused by chronic
inflammation of the airways and lung parenchyma that develops in response to
environmental insults, including cigarette smoke, and manifests clinically with
symptoms of cough, dyspnea on exertion, and wheezing. Patients with COPD
usually live a number of years with progressive disability and multiple acute
exacerbations. Thus, the physician is likely to become involved for many years
in the assessment, treatment, and education of a patient with COPD.
 |
| INTERRELATIONSHIPS OF CHRONIC BRONCHITIS AND EMPHYSEMA |
SUBTYPES
COPD is a
disorder that is characterized by slow emp- tying of the lung during a forced
expiration (see Plate 4-39). In practice, this is measured as the ratio of
forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC), and
the arbitrary definition of airflow obstruction is generally taken to be an
FEV1/FVC ratio lower than 0.70. Because the rate of emptying of the lung
decreases with advancing age, many elderly individuals demonstrate airflow
obstruction even in the absence of a clinical diagnosis of COPD. The diagnosis
of COPD usually describes individuals who have chronic airflow obstruction
associated with tobacco smoke or some other environmental insult, although
aging of the lung has many features that are similar to those of COPD.
COPD encompasses
several clinical subtypes, including chronic bronchitis, emphysema, and some
forms of long-standing asthma. Chronic bronchitis is defined by cough and
sputum production for at least 3 months of the year for more than 2 consecutive
years in the absence of other kinds of endobronchial disease such as
bronchiectasis. In practice, though, most patients with chronic bronchitis have
perennial chronic productive coughs that are dismissed as “smokers’ cough.” Emphysema
is defined as enlargement of the distal airspaces as a consequence of
destruction of alveolar septa. The resultant loss of elasticity of the lung
(i.e., increased distensibility) causes slowing of maximal airflow,
hyperinflation, and air trapping that are the pathophysiologic hallmarks of COPD.
Asthma is defined by completely reversible airflow obstruction and airway
hyperresponsiveness. Chronic persistent asthma may lead to irreversible airflow
obstruction and a subset of those with asthma smoke and have incompletely
reversible airflow obstruction, resulting in a population that meets the
definition of COPD. Because most patients have
features of
more than one subtype and because the treatment approaches are similar,
physicians and epidemiologists usually do not distinguish among the various subcategories
of COPD. In the future, however, as molecular and imaging methods permit finer
distinction of COPD subgroups, it may be possible to more precisely tailor
treatments and define prognosis for individual patients.
Patients
with COPD often seek medical attention after their disease is already severe.
Typically, patients have incurred several decades of damage caused by cigarette
smoking before they experience dyspnea limiting their functional capacity.
Patients may be treated for recurrent lower respiratory tract infections before
a diagnosis of COPD is considered. Clinical presentations vary in the severity
of the underlying lung disease, the rate of progression of disease, and the frequency
of exacerbations.
EPIDEMIOLOGY
COPD is the
fourth leading cause of death in the United States, and mortality related to
COPD is projected to increase as cigarette smoking increases in developing
countries. COPD is also among the leading causes of chronic medical disability
and health care costs in the United States. Morbidity and mortality attributable
to COPD have continued to increase, in contrast with other chronic diseases.
COPD accounts for a great burden of health care costs, including direct costs
of health care and indirect costs related to missed work and caregiver support.
Historically, COPD was described as a disease that predominantly affected white
men. However, the prevalence of COPD among women and minorities has grown in
recent decades as the rate of increase in white men has leveled off. In the
United States, morbidity and mortality from COPD in women now exceeds in men,
which is largely attributable to increases in the prevalence of cigarette
smoking among women. The most rapid increase in COPD mortality is among elderly
women. In developing nations, indoor burning of biomass fuel has been an
important risk factor for COPD among women. As tobacco use has become more
widespread in the developing world, the prevalence of COPD has risen among both
men and women (see Plate 4-28).
RISK
FACTORS
COPD is
caused by a combination of environmental exposures and genetic susceptibility.
1-Antitrypsin deficiency is the best documented genetic risk factor for COPD
and demonstrates the interaction between genetic predisposition and
environmental exposures that results in clinical manifestations of COPD. Other
genetic associations have been suggested but are not as well substantiated.
Inhalational exposures are the major environmental risk factor for COPD, and
cigarette smoking is by far the most common risk factor world-wide. Other
inhalational exposures include outdoor atmospheric pollution and indoor air
pollution from heating and cooking, especially with the use of biomass fuels in
developing countries. Occupational exposures and recurrent bronchial infections
have also been implicated as pathogenic factors. Socioeconomic status and poor
nutrition are other factors that may predispose individuals to developing COPD,
and individuals with reduced
maximal lung function in early life are more likely to develop COPD later in
life.
NATURAL
HISTORY
COPD is a
heterogeneous disorder with the unifying feature of incompletely reversible
airflow obstruction, demonstrated by slow emptying of the lungs during a forced expiration. The
natural history of the decline in FEV1 in patients with COPD was described by
Fletcher and Peto (see Plate 4-28). These investigators reported that most
cigarette smokers have a relatively normal rate of decline in FEV1 with aging,
but a certain subset of smokers is especially susceptible to cigarette smoke,
as demonstrated by an accelerated rate of FEV1 decline. More recent studies
have confirmed that normal nonsmoking adults lose
FEV1 at a rate of 30 mL per year, a consequence of aging-related loss of
elastic recoil of the lung. Studies of patients with COPD show an average
annual decline of FEV1 of 45 to 69 mL per year. Smokers that quit may revert to
the normal state of decline (Plate 4-28). Persons who develop COPD may start
early adulthood with lower levels of lung function and have increased rates of
decline. The decline in lung function is asymptomatic for a period of years,
and patients adjust their activities to limit strenuous exercise. In middle
age, the onset of an intercurrent respiratory infection, ascent to altitude, or
progression of the disease beyond a critical threshold may lead to impairment
of routine daily activities or even acute respiratory failure. These events
lead the patients with COPD to seek medical attention. Thus, the onset of COPD
may appear precipitous even though it is the cumulative result of decades of
progression.
CLINICAL
FEATURES
COPD is a
heterogeneous disease that presents with a spectrum of clinical manifestations.
Although end-stage COPD has classically been described as having features
typical of emphysema or chronic bronchitis, most patients have features of both
(see Plates 4-28 to 4-31). Although COPD represents a spectrum of clinical
presentations, the presence of airflow limitation is a unifying feature, and
spirometry serves as a diagnostic tool and a means of assessing disease
severity (see Plates 4-39 and 4-42). Patients typically have some degree of
dyspnea and may also experience cough and wheezing. COPD is progressive, and
symptoms and clinical features worsen over time despite available treatments.
PREDOMINANCE
OF EMPHYSEMA
The classic
representation of a patient with a predominance of emphysema is an asthenic
patient with a long history of exertional dyspnea and minimal cough productive
of only scant amounts of mucoid sputum (see Plate 4-29). Weight loss is common,
and the clinical course is characterized by marked, progressive dyspnea. On
physical examination, the patient appears distressed and is using accessory
muscles of respiration, which serve to lift the sternum in an anterior-superior
direction with each inspiration. The sternomastoid muscles are well-developed,
but the limbs show evidence of muscle atrophy. The patient has tachypnea, with
relatively prolonged expiration through pursed lips, or expiration is begun
with a grunting sound. Patients who have active grunting expiration may exhibit
well-developed, tense abdominal musculature.
The
hyperinflation of the chest leads to widening of the costal angle of the lower
ribcage and elevation of the lateral clavicles. The flattened diaphragm causes
the lateral ribcage to move inward with each breath. While sitting, the patient
often leans forward, extending the arms to brace him or herself in the
so-called “tripod” position. Patients who brace themselves on their thighs may
develop hyperkeratosis of the upper thighs. The neck veins may be distended
during expiration, yet they collapse with inspiration. The lower intercostal
spaces and sternal notch retract with each inspiration. The percussion note is
hyperresonant, and the breath sounds on auscultation are diminished, with
faint, high-pitched crackles early in inspiration, and wheezes heard in
expiration. The cardiac impulse, if visible, is seen in the subxiphoid regions,
and cardiac dullness is either absent or severely narrowed. The cardiac impulse
is best palpated in the subxiphoid region. If pulmonary hypertension is
present, a murmur of tricuspid insufficiency may be heard in the subxiphoid
region.
The minute
ventilation is maintained, the arterial Po2 is often above 60 mm Hg, and the
Pco2 is low to normal. Pulmonary function testing demonstrates an increased
total lung capacity (TLC) and residual volume (RV), with a decreased vital
capacity. The DLCO (diffusing capacity for carbon monoxide) is decreased,
reflecting the destruction of the alveolar septa causing reduction of capillary
surface area. When the DLCO decreases below 50% predicted, many patients with
emphysema have arterial oxygen desaturation with exercise.
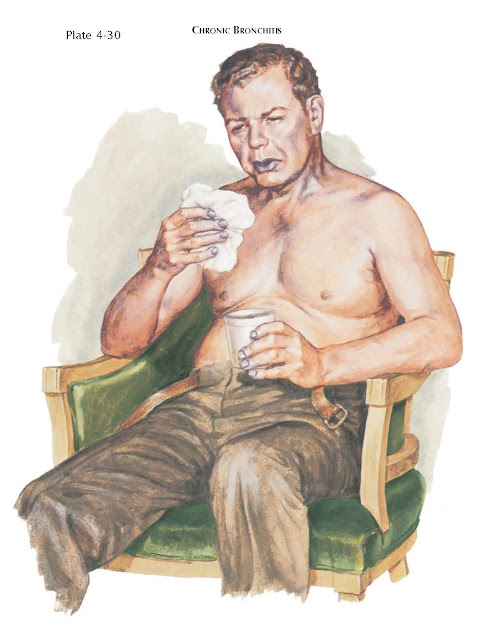
PREDOMINANCE
OF CHRONIC BRONCHITIS
Patients
with a predominance of chronic bronchitis typically have a history of cough and
sputum production for many years along with a history of heavy cigarette
smoking (see Plate 4-30). Initially, the cough may be present only in the
winter months, and the patient may seek medical attention only during the more
severe of his or her repeated attacks of purulent bronchitis. Over the years,
the cough becomes continuous, and episodes of illness increase in frequency,
duration, and severity. After the patient begins to experience exertional
dyspnea, he or she often seeks medical help and is found to have a severe
degree of obstruction. Frequently, such patients do not seek out a physician
until the onset of acute or chronic respiratory failure. Many of these patients
report nocturnal snoring and daytime hypersomnolence and demonstrate sleep
apnea syndrome, which may contribute to the clinical manifestations.
Patients
with a predominance of bronchitis are often overweight and cyanotic. There is
often no apparent distress at rest; the respiratory rate is normal or only
slightly increased. Accessory muscle usage is not apparent. The chest
percussion note is normally resonant and, on auscultation, one can usually hear
coarse rattles and rhonchi, which change in location and intensity after a deep
breath and productive cough. Wheezing may be present during resting breathing
or may be elicited with a forced expiration.
The minute
ventilation is either normal or only slightly increased. Failure to increase
minute ventilation in the face of ventilation-perfusion mismatch leads to
hypoxemia. Because of impaired chemosensitivity, such patients do not
compensate properly and permit hypercapnia to develop with Paco2 levels above
45 mm Hg. The low Pao2 produces desaturation of hemoglobin, which causes
hypoxic pulmonary vasoconstriction and eventually irreversible pulmonary
hypertension. Desaturation may lead to visible cyanosis, and hypoxic pulmonary
vasoconstriction leads to right-sided heart failure (see Plate 4-32). Because
of the chronic systemic inflammatory response that occurs with COPD, these
patients often do not have a normal erythrocytic response to hypoxemia, so the
serum hemoglobin may be normal, elevated, or even decreased.
The TLC is
often normal, and the RV is moderately elevated. The vital capacity (VC) is
mildly diminished. Maximal expiratory flow rates are invariably low. Lung
elastic recoil properties are normal or only slightly impaired; the DLCO is
either normal or minimally decreased.
PATHOLOGY
Large
Airways Disease (see Plate 4-33)
Chronic bronchitis
is associated with hyperplasia and hypertrophy of the mucus-secreting glands
found in the submucosa of the large cartilaginous airways. Because the mass of
the submucous glands is approximately 40 times greater than that of the intraepithelial goblet cells, it is
thought that these glands produce most airway mucus. The degree of hyperplasia
is quantitatively assessed as the ratio of the submucosal gland thickness to
the overall thickness of the bronchial wall from the cartilage to the airway lumen.
This ratio is known as the Reid index. Although the Reid index is often
low in the bronchi of patients who do not have symptoms of COPD during life and
is frequently high in those with chronic bronchitis, there is sufficient overlap
of Reid index values to suggest that a gradual change in the submucous glands
may take place. Thus, the sharp distinction of the clinical definition of
chronic bronchitis cannot correlate completely with the pathologic changes
in large airways. Although patients with chronic mucus hypersecretion with
cough and sputum are more prone to respiratory infections and exacerbations of
COPD, the presence of cough and sputum are not, by themselves, indicative of a
poor prognosis in the absence of airflow obstruction. The magnitude of airflow
obstruction is better correlated with the pathologic involvement of the small
airways.
Small
Airways Disease (see Plate 4-33)
COPD is also
associated with changes in the small airways, those less than 2 mm and between
the fourth and twelfth generation of airway branching in the lungs. The changes
in the small airways may occur independently of changes in the larger airways.
Changes in the small airways occur across a spectrum and may range from bland
intraluminal secretions to a more cellular infiltrate, with polymorphonuclear
neutrophils, macrophages, CD4 cells and other lymphocyte subtypes. The presence
of lymphoid follicles in the small airways demonstrates increased immune
surveillance of the mucosal surface. In addition to cellular inflammation, airway
wall thickening, including changes in the epithelium, lamina propria, and
adventitia, corresponds to disease progression. The diffuse changes in small
airways con- tribute more to the obstruction and maldistribution of inspired
gas than do the abnormalities in large airways. Obstruction of small airways
with mucous plugs is associated with increased mortality.
EMPHYSEMA
The several
types of emphysema are classified according to patterns of septal destruction
and airspace enlargement within terminal respiratory units, or acini (see
Plates 4-34 to 4-36). The normal acinus is supplied by a terminal
bronchiole. The terminal bronchiole undergoes three orders of branching first into respiratory
bronchioles with alveolated walls, into alveolar ducts, and finally
into alveolar sacs.
If the
septal destruction and dilatation are limited to the central portion of the
acinus in the region of the terminal bronchiole and respiratory bronchioles,
the disorder is called centriacinar or centrilobular emphysema (see
Plate 4-35). Because of septal destruction, there is free communication between
all orders of respiratory bronchioles. Alveolar sacs at the periphery of the
acinus lose volume as the central portions enlarge. Although centriacinar
emphysema is often considered to be a diffuse disease process, there is
considerable variation in severity from acinus to acinus within the same segment or lobe. In
general, however, more of the acini are affected in the upper lung zones than
in the lower zones. Extensive centriacinar emphysema is most often found in
those with histories of heavy smoking and chronic bronchitis.
In contrast
to centriacinar emphysema, panacinar or panlobular emphysema affects
the acinus more uniformly with less variability within an individual segment or
lobe (see Plate 4-36). There is some tendency for the lower zones to be more
severely affected. Panacinar emphysema is the characteristic lesion in 1-antitrypsin deficiency,
although smokers with 1-antitrypsin deficiency may have centriacinar emphysema
as well. Panacinar emphysema to a mild degree is a common finding after the fifth
decade of life and may be extensive in elderly nonsmoking patients who have
age related “senile” emphysema. In severe smoking-related chronic obstructive
airway disease, both centriacinar and panacinar emphysema are ordinarily found
along with chronic bronchitic
changes in the airways.
When alveolar wall destruction is restricted to the periphery of the
acinus, most often in regions just beneath the visceral pleura, the disorder is
designated paraseptal emphysema. This form leads to development of
subpleural bullae that may result in episodes of spontaneous pneumothorax in
otherwise healthy young adults.
PATHOBIOLOGY
COPD is
characterized by chronic inflammation in the peripheral airways and the lung
parenchyma (see Plates 4-37 and 4-38). The predominant cells are macrophages,
CD8 lymphocytes, and neutrophils. The inflammatory mediators leukotriene B4,
tumor necrosis factor- (TNF-), and interleukin-8 (IL-8) are increased in the
sputum of patients with COPD and may play an important role. An imbalance
between proteases and antiproteases is also likely to be important in the
pathogenesis of COPD (see Plate 4-38). Macrophages and neutrophils release many
different proteases that break down connective tissue, such as elastin, in the
lung parenchyma. The proteases may induce direct destruction of lung tissue as
well as trigger cascades of intracellular events that lead to apoptotic cell
death. Moreover, proteases are potent promoters of mucus cell metaplasia and
mucus cell secretion, contributing to chronic bronchitis. Neutrophil elastase,
proteinase 3, and cathepsins all produce emphysema in laboratory animals.
Neutrophil elastase is inhibited by 1- antitrypsin and deficiency of this
enzyme is the pre-dominant contributor to the emphysema in those with the
severe genetic defect. Matrix metalloproteinases (MMPs) from macrophages and
neutrophils may also have a key role in inducing emphysema. In the normal
state, proteolytic enzymes are counteracted by antiproteases such as
1-antitrypsin and serum leukocyte proteinase inhibitor (SLIPI). By inducing
inflammation, smoking increases release of proteases in the terminal airspaces
in patients in whom COPD develops. More- over, smoking may also inactivate
antiproteases via MMP inhibition of 1-antitrypsin, which itself is an
inhibitor of a protease that counteracts the actions of MMPs. By reducing
1-antitrypsin’s inhibition of this protease, known as tissue inhibitor of
metalloproteinases (TIMP), the actions of MMPs are enhanced. Smoking also leads
to increased reactive oxygen species (ROS), which can promote inflammatory gene
transcription by breakdown of the inhibitor of the transcription factor nuclear
factor kappa-B (NFB), known as IN-KB. ROS can also inactivate histone
deacetylase (HDAC), leading to increased DNA acetylation and gene transcription.
Furthermore, CD8+ cells can promote macrophage production of MMPs through
interferon-inducible cytokines, such as inducible protein of 10kD (IP-10),
interfection-inducible T-cell alpha chemoattractant (l-TAC), and monokine
induced by interferon-gamma (MIG). Thus, an insufficient concentration of
antiproteases may result in parenchymal damage.
Oxidative
stress may also contribute to the injury characteristic of COPD by oxidation of
proteins, cell membranes,
and nucleic acids, triggering a cellular stress response that ultimately leads
to apoptotic cell death. The inflammation in COPD is not only localized to the
lungs but is present on a systemic basis. Patients with COPD have elevated
concentrations of C-reactive protein and interleukin-6, even during times of
stable symptoms. Weight loss and muscle atrophy in COPD have been associated
with increased circulating levels of TNF-and soluble TNF-receptors.
The final common pathway
of inflammatory cytokines, protease-antiprotease imbalance, and oxidative stress
is destruction of alveolar epithelial and capillary endothelial cells by a
programmed sequence of cell death, or apoptosis. Because the lung requires
replacement of its cellular scaffolding on a continuing basis, any process that
leads to an imbalance of cell destruction and cell growth can eventually lead
to emphysema. Thus, insufficiency of growth factors is also postulated to
contribute to the development of emphysema.
The presence
of CD8 cells and airway-associated lymphoid follicles in the lung parenchyma in
smokers with COPD has raised the possibility that immunologic processes such as
autoimmunity or response to chronic viral infection may also contribute to the
pathogenesis of COPD.
α1-ANTITRYPSIN
Serum levels
of α1-antitrypsin are either deficient or absent in some patients with early
onset of emphysema associated with particular genotypes (see Plate 4-38). Most
people in the normal population have α1-antitrypsin levels in excess of 250
mg/100 mL of serum along with two M genes, designated as Pi-type MM. Several
genes are associated with alterations in serum α1-antitrypsin levels, but the
most common ones associated with emphysema are the Z and S genes. Individuals
who are homozygous ZZ or SS have serum levels of α1-antitrypsin of less than 50
mg/100 mL and develop severe panacinar emphysema at an early age, particularly
if they smoke or are exposed to occupational dusts. The MZ and MS heterozygotes
have intermediate levels of serum α1-antitrypsin. Although smokers with MZ or
MS genotypes may have slightly increased decline in FEV1 if they smoke, the
risk of developing COPD is not materially increased beyond other smokers.
α1-antitrypsin deficiency is caused by a single amino acid substitution. The Z mutation is caused by a glutamate to lysine
mutation at position 342, and the S mutation is caused by a glutamate to valine
mutation at position 264. These mutations lead to misfolding of the protein
preventing release from the liver, where it is mainly manufactured. The
misfolded protein may be destroyed by proteosomal processes, or if it
polymerizes, may be stored in the endoplasmic reticulum and not released into
the circulation. Excessive liver storage may lead to inflammatory liver disease
and cirrhosis, particularly in affected infants and children.
The precise
way that antitrypsin deficiency produces emphysema is unclear. In addition to
inhibiting trypsin,α1-antitrypsin effectively inhibits elastase and
collagenase, as well as several other enzymes. α1-antitrypsin is an acutephase
reactant, and the serum levels increase in association with many inflammatory reactions and with estrogen
administration in all except homozygotes. It has been proposed, with some
supporting experimental evidence, that the structural integrity of lung elastin
and collagen depends on this antiprotease, which protects the lung from
proteases released from leukocytes. Proteases released by lysed leukocytes in
the alveoli may be uninhibited and consequently free to damage the alveolar
walls themselves. Alternative theories suggest that the unopposed protease activity may lead to an
ongoing immune-mediated inflammatory response or acceleration of natural
programmed cell death.
PATHOPHYSIOLOGY
Whether
bronchitis or emphysema predominates, by the time a patient with COPD begins to
have symptoms, airflow
limitation is readily demonstrable as an obstructive ventilatory defect. The
most easily measured indexes of obstruction are taken from the volume-time plot
of a forced expiratory VC maneuver, classically measured with a spirometer
coupled to a rotating drum kymograph. Although volume-measuring spirometers are
stable, rugged, and linear instruments, most modern spirometry systems use
flow-measuring devices (pneumotachometers) interfaced with a microprocessor that
integrates flow over time to produce a time-based record of forced expired
volume (see Plate 4-39). The FEV1 is low both as a percentage of the value predicted
for a given gender, age, and height category and as a percentage of the
patient’s own FVC. Depending on the purpose of the pulmonary function test, an
obstructive ventilatory defect is defined either as an FEV1/FVC ratio of less
than 70% or less than the 95th percentile for the demographic category.
With COPD,
static lung volumes are often abnormal. Plate 4-39 depicts the normal lung
volumes and those often found in COPD. The functional residual capacity (FRC)
is the lung volume at the end of a quiet exhalation and, in normal subjects, is
the volume at which the inward recoil of the lung is equal and opposite to the
outward recoil of the relaxed chest wall. An elevated FRC in individuals
with COPD results from the loss of the static elastic recoil properties of the
lung as well as initiation of inspiration before the static balance volume is
reached (so-called “dynamic hyperinflation”). TLC is determined by pressures
exerted by the diaphragm and muscles of the chest wall in relation to the
static elastic recoil properties of both the chest wall and lung. When TLC is
elevated in COPD, a significant degree of emphysema is present, although the TLC
can also be elevated during acute episodes of asthma. RV is elevated early in
the clinical course of COPD and is a sensitive sign of airflow limitation. Early
in the course of the disease, elevation of RV is thought to be caused by
closure of airways, but late in the disease, emphysematous bullae may also
contribute to the elevation in RV. Because the TLC does not increase as much as
the RV increases, the VC (i.e., TLC RV) decreases with advancing COPD.
The
measurement of static lung volumes in COPD is subject to some technical issues (see Plate 2-3). Resident gas
methods using helium dilution or nitrogen may underestimate the true lung
volumes because of incomplete gas mixing or washout in regions with impaired
ventilation. Plethysmographic lung volumes that depend on Boyle’s law relying
on the compressibility of resident gas in the lung are more accurate but are
subject to overestimation of the true lung volume if the panting frequency is
too rapid to permit equilibration of the mouth and alveolar pressures. Because
the difference between the resident gas and plethysmographic measure is caused by
regions of lung with little or no ventilation, the difference between the two
methods has been called “trapped gas” and used as an indicator of COPD severity
(see Section 2).
In addition
to the easily demonstrable obstructive abnormalities during forced exhalation,
there are significant alterations in the pressure-flow relationships during
ordinary breathing in COPD. This contrasts with exhalation in normal subjects
who can increase expiratory
flow during tidal breathing (see Plate 4-39). Because of the slow emptying of the
lung in COPD, the next breath is initiated before the respiratory system can
return to the static FRC. This means that the individual breathes at higher
lung volumes to maintain adequate expiratory airflow, a condition referred to as
dynamic hyperinflation (see Plate 4-39). Although breathing at high lung
volumes has the advantage of increasing airflow because of the increased lung
elastic recoil, it requires an increase in the work of
breathing and a decrease in the efficiency of breathing. Increasing respiratory
rate accentuates dynamic hyperinflation and can worsen the sensation of dyspnea.
Pursed-lip breathing causes patients to slow their respiratory rate and can
relieve dyspnea by diminishing dynamic hyperinflation.
The
physiologic hallmark of emphysema is a reduction in lung elastic recoil caused
by destruction of alveolar septal elements. This causes the pressure-volume
curve of the lung to be shifted upward and to the left, resulting in decreased
static recoil pressure at a specific lung volume and an increase in the
compliance of the lung (see Plates 4-39 and 4-40).
The surface
area of the alveolar-capillary membrane is reduced as a consequence of
emphysema. This results in decreased transfer of diffusion-limited gases such
as carbon monoxide across the alveolar-capillary membrane. This is measured
in the pulmonary function laboratory as the DLCO. The DLCO correlates roughly
with the magnitude of reduction in maximum elastic recoil of the lung as well
as the anatomic extent of emphysema assessed by imaging with computed
tomography (CT). In chronic bronchitis, the DLCO may be preserved, and in
asthma, the DLCO tends to be elevated.
With the
progression of COPD comes progressive exercise limitation. This is caused by
the increased work of breathing as ventilation increases with exercise. With
increased respiratory rate, patients develop dynamic hyperinflation, a condition
in which the end-expiratory lung volume does not return to the static end-
expiratory volume of FRC (see Plate 4-40). The hyper- inflation that occurs
causes an increased work of breathing and exacerbates dyspnea. An indicator of
dynamic hyperinflation is the inspiratory capacity (IC), which progressively
decreases with increasing ventilation. Measures that reduce dynamic
hyperinflation, increasing IC, can improve exercise capacity. These include
alterations in breathing pattern, oxygen supplementation, helium inhalation,
and use of inhaled bronchodilators, particularly long-acting, and lung volume
reduction surgery.
RADIOGRAPHIC
APPEARANCE
Chronic
Bronchitis
On plain
chest radiographs, thickening of bronchial walls is often seen as parallel or
tapering shadows, referred to as tram tracking or ring shadows of
airways that are visualized in cross-section. A generalized increase in lung
markings at the bases is also frequently seen and is referred to as dirty
lungs. In patients who have been exposed to occupational dusts, these
markings may be accentuated but do not necessarily indicate the presence of
pneumoconiosis.
The CT may
show airway wall thickening or mucoid impactions in patients with COPD even in
the absence of emphysema. The magnitude of these abnormalities, however, does
not necessarily correlate with the severity of airflow obstruction or the extent
of emphysema, and it remains to be seen whether there are prognostic or
therapeutic implications of these findings.
Emphysema
In
evaluating plain radiographs, a range of findings can represent emphysema. These
include attenuation of the pulmonary vasculature peripherally, irregular
radiolucency of lung fields, flattening or inversion of the diaphragm as seen on
both posteroanterior (PA) and lateral projections, and an increase in the
retrosternal space on the lateral projection. The latter two findings have correlated best with the severity of emphysema as
assessed at subsequent postmortem examination.
High-resolution
CT examination of the chest is now considered the best indicator of the extent
and distribution of emphysema (see Plate 4-41). Qualitative visual assessments
can assess the presence of thin-walled bullae and regions of diminished
vascularity. Quantitative assessments use the degree of attenuation of x-rays
to estimate the air-tissue ratio as a measure of airspace enlargement. Regions
of the lung on thinsection CT scans that approach the radiodensity of air
(1000 Hounsfield units [HU]) are considered to be emphysema. For example, the
emphysema index is calculated as the percentage of image voxels in the lung
regions that have a density 950 HU). Other methods rely on the statistical
distribution of lung densities, quantifying the severity of emphysema by the
lung density at the lowest 15th percentile of voxels.
MANAGEMENT
Patient
Education
Educating
patients about the chronic nature of their disease and preventive measures is
an important, ongoing process that will not be completed in one visit. The
health care provider should focus on topics that are most pertinent to the
needs of the patient and to the stage of disease. Topics that should be covered
include the nature and prognosis of COPD, proper use of inhalers and adherence
to medications, role of exercise and pulmonary rehabilitation, nutrition, and
use of supplemental oxygen. Providing written materials in addition to
office-based education is beneficial. Special counseling is needed for patients
with α1-antitrypsin deficiency and their family members to determine whether
genetic testing is necessary or desired. For those with advanced disease,
discussions about end-of- life planning and advance directives regarding life
support is often welcomed by patients and facilitates communication between the
patient and his or her family.
PREVENTIVE
MEASURES
Smoking
Cessation
Smoking
cessation is the single most effective intervention to slow the progression of
COPD. and should be a primary goal emphasized by physicians caring for COPD
patients. A smoking history should be obtained at each patient encounter. For
patients who smoke, a direct, unambiguous, and personalized smoking cessation
message should be given by the physician. Assistance with pharmacologic
adjuncts and referral to more intensive smoking counseling groups should be
offered. A combination of counseling and pharmacotherapy, including nicotine
replacement therapy, varenicline, and bupropion, has been shown to be the most
effective means of achieving smoking cessation. Guidelines recommend
comprehensive tobacco control programs with consistent, clear, and repeated
nonsmoking messages that are delivered at every medical encounter.
The Lung
Health Study demonstrated the impact of smoking cessation in a landmark trial
of more than 5800 smokers
with spirometric signs of early COPD who were randomly assigned to smoking
intervention plus placebo, smoking intervention plus bronchodilator, or no
intervention. Randomization to the smoking cessation intervention was shown to
reduce the rate of decline in FEV1 and to improve mortality, mainly related to
cardiovascular disease and lung cancer. Throughout the study, some patients
reverted from being smokers to
quitters and vice versa. When patients were followed for 11 years, those who
successfully quit smoking had a small initial increase in FEV1 followed by a
slow, normal rate of FEV1 decline. Quitters who reverted to cigarette smoking
showed a more rapid FEV1 decline than those who were sustained quitters. At
14.5 years, those randomized to the 10-week smoking cessation had a reduced
mortality rate compared with those randomized to usual care.
Persons who
quit smoking with earlier disease have better outcomes relative to those who
continue to smoke than those who quit smoking later in the disease. When the
disease is advanced, the inflammatory response persists, and the rate of decline
of lung function tends to progress. Because there are many years of
asymptomatic decline in lung function, it is possible to diagnose COPD with
forced expiratory spirometry before the disease is apparent and to implement
aggressive smoking intervention programs. There is no consensus whether it is
necessary to screen for COPD among all cigarette smokers, but there is evidence
that presentation of a person’s FEV1 in terms of “lung age” does assist in
smoking cessation.
Reduce
Harmful Environmental Exposures
Reduction of
secondhand smoke and other environmental pollutants is important in preventing
the progression of COPD. Reducing exposure to indoor and outdoor pollutants
requires a combination of public policy to define and uphold air quality
standards and steps taken at the individual level to minimize exposure to
elevated concentrations of pollutants in the indoor or outdoor environments.
Occupational exposures should be ascertained with attention to fumes and dusts,
and vigorous measures should be taken to eliminate harmful exposures.
Respiratory protective equipment should be worn by COPD patients exposed to
heavy dust concentrations. Although there is no level of FEV1 that absolutely
prohibits the use of respiratory protective equipment, some COPD patients will
need to change their work environment if they cannot tolerate protective
devices.
Minimize
Infectious Risks
Although it
is not possible to completely eliminate exposure to the many infectious agents,
patients should keep away from large crowds and persons with obvious
respiratory infections, especially during influenza season. Handwashing or hand
sanitization should be emphasized.
Patients should be educated about early signs of exacerbations and
treated promptly. Some patients may want to keep a prescription or supply of
antibiotics or steroids available at home. Pneumococcal vaccination is
recommended, although the evidence of its particular efficacy in COPD is lacking. Annual influenza immunization
can prevent or attenuate this potentially fatal infection.
Exercise
and Rehabilitation
Regular,
prudent, self-directed exercise is recommended for all individuals with COPD to
prevent the muscle deconditioning that often accompanies the disorder. Individuals
should be encouraged to perform at least 20 to 30 minutes of constant
low-intensity aerobic exercise such as walking at least three times per week.
This is usually feasible even in more severely impaired patients. It is
important to instruct patients that they should exercise to a level of dyspnea
that is tolerable for the entire exercise period. Supplemental oxygen for
exercise is necessary for patients who desaturate with exercise and may benefit some patients
without demonstrable oxygen desaturation in terms of exercise capacity and
training effect.
Formal rehabilitation
programs are established as an effective component of COPD management and
should be offered to patients who have substantial limitation in daily
activities (see Plate 5-11). The goals of pulmonary rehabilitation are to
improve quality of life, reduce symptoms, and increase physical and emotional
participation in daily activities. To achieve these goals, pulmonary
rehabilitation programs use a multidisciplinary approach, including exercise
training, nutrition, education, and psychological support. Smoking cessation
programs are often linked to pulmonary rehabilitation programs. Exercise
training typically consists of bicycle ergometry or treadmill exercise. Upper
extremity weight training is often included as a component of strength
training. Practical advice on energy conservation and pacing during activities
of daily living can be delivered individually or in group sessions. Proper use
of inhalers, oxygen supplementation, and good nutrition are goals of education
programs.
TREATMENT
OF STABLE CHRONIC OBSTRUCTIVE PULMONARY DISEASE
The goals of
treatment of COPD are to prevent progression and complications of the disease,
relieve symptoms, improve exercise capacity, improve quality of life, treat
exacerbations, and improve survival. In addition to smoking intervention and
treatment of hypoxemia with supplemental oxygen, pharmacologic therapy is
available for treatment of patients with COPD. See the section on pharmacology
(Plates 5-1 to 5-10) for a more detailed description of many of the drugs discussed
below.
The current
goals of drug therapy are not only to improve lung function, but also to
improve quality of life and exercise capacity and to prevent exacerbations. The
recommended approach to drug treatment for COPD is to sequentially add agents using
the minimum number of agents and the most convenient dosing schedule, starting
with the agents having the greatest benefit, best tolerance, and lowest cost
(see Plate 4-42).
Inhaled
bronchodilators, including-agonists and anticholinergic agents, are the
foundation of treatment for patients with COPD. They are given on a regular
basis to maintain bronchodilation and on an as-needed basis for relief of
symptoms. Both-agonist and anti-cholinergic classes are available in
short-duration (4-6 hour) and long-duration (12-24 hour) forms. Evidence
suggests that long-acting agents are more effective than short-acting agents,
but the choice of medication
should also account for cost considerations and patient preference. Combination
of different classes of bronchodilators is often more effective than increasing
the dose of a single agent, and combination inhalers can simplify treatment
regimens. Individuals with frequent exacerbations or more severe COPD may
benefit from a combination inhaler of corticosteroids and long-acting
bronchodilator. Long-acting oral theophylline can also be used as adjunctive
therapy. Chronic use of systemic
corticosteroids should be reserved for individuals with very frequent or
life-threatening exacerbations who cannot tolerate their discontinuation.
Replacement
therapy with α1-antitrypsin should be considered for individuals with severe
deficiency. Observational studies suggest that individuals with moderate degrees
of impairment (FEV1 35%-65% predicted) seem to benefit most in terms of preservation of lung function and
improved survival.
Patient education about pharmacotherapy is important
to ensure proper use of medications, as well as to enhance adherence. Inhaled
agents are administered by metered-dose inhalers or dry powder inhalers or as a
nebulized solution. The selection of route of administration is made by cost
and convenience of the device because all are similarly effective if used
properly. Proper use of inhaled medications is difficult for many patients to
learn and retain. Adherence with inhaled medication, particularly when it does
not provide immediate symptom relief, is poor. Typically, about half of
patients do not take their medication in the dose or quantity prescribed.
Reasons for this include a lack of understanding of the role of the medication,
failure of the medication to provide meaningful benefit, complexity of the
treatment program, and expense of the treatment. Many patients do not want to
confide poor adherence to their physician, so it is important for the physician
to ascertain this information in a way that does not interfere with the
relationship with the patient. If nonadherence is a problem, the treating
physician can undertake actions to improve adherence such as simplification of
the medication program, education about the benefits of treatment, linking drug
use to established habits such as meals or tooth brushing, or prescribing less
costly drugs.
TREATMENT
OF EXACERBATIONS
COPD
exacerbations are characterized by worsening dyspnea, cough, and increased
sputum production. There are several formal definitions of a COPD exacerbation,
but a useful working definition is that a COPD exacerbation is a worsening of
dyspnea, cough, or sputum production that exceeds day-to-day variability and
that persists for more than 1 or 2 days. On average, patients with COPD have
two to three exacerbations per year, but there is wide variation, and the
frequency of exacerbations is only roughly correlated with severity of airflow
obstruction. The best predictor of future exacerbations is a history of
frequent exacerbations, and these are more common in patients with chronic
cough and sputum production. Precipitating events include respiratory and
nonrespiratory infections; exposure to respiratory irritants and air pollution;
and comorbid conditions such as heart failure, pulmonary embolism, myocardial
ischemia, or pneumothorax.
For patients
treated at home, increasing the frequency and intensity of inhaled short-acting
bronchodilators for several days is effective in mild exacerbations. A
nebulizer may be needed for those who have difficulty using inhalers or in those
with severe dyspnea. Increasing dyspnea accompanied by a change in the quantity
or color of phlegm is usually an indication of bacterial infection and should
prompt initiation of antibiotics. A course of corticosteroids, equivalent to 30
to 60 mg of prednisone for 7 to 14 days, will shorten the duration of symptoms
for patients with exacerbations managed as outpatients.
For patients
admitted to the hospital, intensification of inhaled bronchodilator treatment,
systemic corticosteroids, and antibiotics should be administered.
Controlled
oxygen supplementation should be provided at the lowest level needed to reverse
hypoxemia and minimize the induction of hypercapnia. The selection of the oral
or intravenous route for antibiotics and corticosteroids is determined by the
severity of the illness and the ability of the patient to tolerate oral
medication.
Treatment in
an intensive care setting should be undertaken for patients with severe
life-threatening exacerbations and those
who require more constant attention. For patients with respiratory failure,
noninvasive mask ventilation has proven to be an effective strategy to avert
endotracheal intubation, shorten the duration of illness, and improve outcomes.
When non-invasive mask ventilation is not successful in sustaining ventilation
or if the patient is too ill to use the mask, endotracheal intubation and
mechanical ventilation are needed to treat respiratory failure. The mechanical
ventilator should be set to provide a provide a prolonged duration of
expiration to minimize dynamic hyperinflation (“intrinsic positive
end-expiratory pressure”), which can lead to dyspnea, ventilator
dyscoordination, and barotrauma. Care should be taken not to overventilate the
patient and cause alkalemia, which may ultimately impede liberation from the
ventilator. Survival after an episode of acute respiratory failure for COPD is
about 50% at 2 years after discharge, with about 50% of the patients being
readmitted to the hospital within 6 months.
TREATMENT
COMPLICATIONS
Patients
with advanced COPD are prone to developing secondary complications of the
disease. The goals of treatment are to restore functional status as quickly and
as much as possible and to alleviate distress and discomfort.
Pneumothorax
Acute
worsening of dyspnea may result from a pneumothorax, which patients with
bullous emphysema are prone to have. Treatment involves use of
highconcentration oxygen and drainage with a catheter or chest tube connected
to a valve or vacuum drainage system. Patients with recurrent,
life-threatening, or bilateral pneumothorax are candidates for pleurodesis to
prevent recurrence.
Cor
Pulmonale
The
pulmonary vascular bed normally has an impressive reserve that accommodates
large increases in cardiac output with minimal elevations of pulmonary artery
pressures (see Plate 4-32). In COPD, there is a decrease in the total
cross-sectional area of the pulmonary vascular bed caused by anatomic changes
in the arteries; constriction of smooth muscle in response to alveolar hypoxia;
and, to the extent that emphysema is present, a loss of pulmonary capillaries.
Therefore, the pressures that must be generated by the right ventricle are
elevated, and dilatation and hypertrophy of the right ventricle result. Overt right
ventricular failure often occurs in association with endobronchial infections,
which leads to worsening hypoxemia and hypercapnia. Such episodes are more
frequent in patients in whom bronchitis is dominant.
Patients
with cor pulmonale are cyanotic
and have distended neck veins that do not collapse with inspiration, hepatic
engorgement with a tender and enlarged liver, and pitting edema of the
extremities. The heart may or may not appear enlarged on a PA chest radiograph,
but pulmonary vessels are prominent. Physical examination may disclose a palpable right ventricular
heave and an audible early diastolic gallop that is accentuated by inspiration.
On occasion, there is dilatation of the tricuspid ring with secondary tricuspid
insufficiency; this disappears with effective treatment. The electrocardiogram
may show changes of right ventricular hypertrophy. Echocardiographic findings
may be inconsistent, especially because of difficulty obtaining good-quality
views of the right ventricle because of overlying hyperinflation of the lungs.
Thus, in patients suspected to have pulmonary hypertension, a right- sided
heart catheterization is the most definitive means of making the diagnosis.
Treatment of
hypoxemia is the mainstay of prevention and treatment of cor pulmonale.
Supplemental oxygen should be prescribed to maintain adequate oxygen
saturations regardless of the development of hypercapnia (see Plates 5-12 to
5-14). The presence of sleep apnea is common in patients with COPD and
pulmonary hypertension. Thus, evaluation with a sleep study is often helpful to
determine the need for nocturnal oxygen or continuous positive airway pressure
(see Plates 4-165 to 4-166). In occasional patients who have severe pulmonary
hypertension with minimal COPD, pulmonary thromboembolism should be ruled out.
Rarely, pulmonary vasodilators may be used when the magnitude of pulmonary
hypertension seems disproportionate to the severity of the COPD and hypoxemia.
SURGICAL
TREATMENT
Lung
Volume Reduction Surgery
(see Plate
5-32)
Lung volume
reduction surgery (LVRS) is a surgical procedure that involves stapled
resection of 20% to 30% of
the lung bilaterally, usually from the apices (see section on LVRS). Although
some patients show sub-stantial physiologic and symptomatic improvement after
LVRS, many do not. The group of patients that fares best with LVRS is those who
have emphysema predominantly in the upper lung zones and who have low exercise
capacity despite pulmonary rehabilitation. These patients have improved survival
after LVRS and show improved functional status and quality of life. Conversely,
patients without upper lobe predominance (i.e., lower lobe emphysema or
homogeneous emphysema) and who have adequate exercise capacity after
rehabilitation have worse outcomes after LVRS.
Surgical
resection of a single large bulla is rarely indicated for treatment of COPD.
Isolated giant bullae are usually the result of an expanding congenital cyst.
The generally accepted indication for resection of a single large bulla is that
it occupies more than one-third of the hemithorax and causes compression of
normal lung. Some believe that a preserved DLCO is an indicator of those most
likely to improve after bullectomy.
Lung
Transplantation (see Plate 5-33)
In younger
patients with advanced disease, lung transplantation should be a treatment
consideration (see Plate 5-33). Criteria for lung transplantation referral in
patients with COPD is an FEV1 below 25% predicted, severe hypercapnia, or
severe pulmonary hyper- tension in patients younger than age 60 to 65 years.
The traditional recommendation is that patients should be referred for
transplantation when their life expectancy is less than 2 years because this is
the average waiting time on a
transplant recipient list. In recent years, the waiting time has lengthened to
closer to 4 years, so this may
influence physicians to make earlier referrals. Other comorbid conditions, such
as poor nutritional status, obesity, chronic mycobacterial infection, or severe
osteoporosis, as well as suboptimal psychosocial support, are considered
relative contraindications. Current smoking, recent malignant disease, major
organ system failure (particularly renal or chronic hepatitis B or C
infections) are considered absolute contraindications. Lung transplantation may
be either unilateral or bilateral depending on the availability of donor organs
and the preference of the transplant surgeon. Generally, younger patients and
those with accompanying bronchiectasis are considered more suitable candidates
for bilateral lung transplantation.
In the past,
COPD has been the most common indication for lung transplantation, accounting
for nearly 40% of all lung transplants and about 50% of single lung
transplants. This is accounted for by the high prevalence of COPD as well as
the better survival rate for patients with COPD than those with other transplant indications while awaiting donor organs. However, current criteria for
prioritization of transplant recipients based on diagnosis rather than waiting
time alone are likely to diminish the likelihood that COPD patients will
receive donor organs. Early survival for patients with COPD after lung
transplant is slightly better than that of other diagnostic groups in the first
few years. Overall, 30-day survival is 9 %, 3-year survival is 61%, and 5-year survival is
45%.