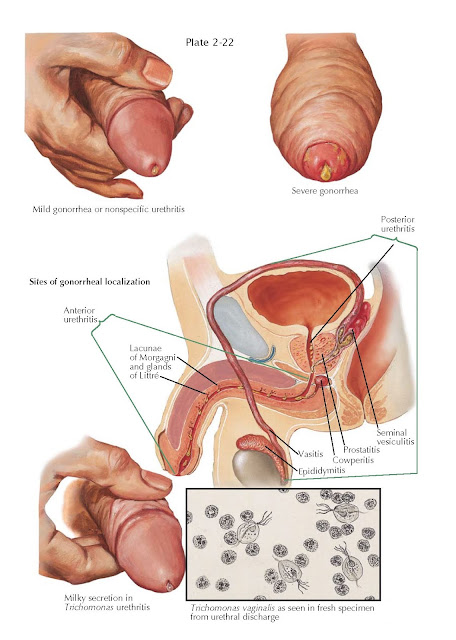
URETHRITIS
Gonorrheal urethritis (Neisseria gonorrhoeae), initially a
sexually transmitted infection of the urethral mucosa, becomes symptomatic
after the gonococci penetrate perimucosal tissues. Crypts and glands of the
penile urethra fill with leukocytes and organisms. Chronic gonorrheal urethritis
results from retention of gonococci in the urethral glands (Littré) and their
intermittent discharge from these glands (carrier stage). The incubation period
of gonorrhea is 3 to 5 days. In mild infections, the urethral discharge may be
scant and often mistaken for nonspecific urethritis.
Abundant purulent discharge
and balanoposthitis (with preexisting phimosis) are typical of severe
infections. In severe cases, the corpus spongiosum may become involved,
resulting in painful erections. With extension of the infection into the
posterior urethra, urinary frequency and dysuria occur. Infection of the
prostate is usually asymptomatic, unless a prostatic abscess is present.
Gonorrhea may spread through the spermatic cord to the vas deferens (vasitis)
and epididymis, resulting in epididymitis. Gonococcal endocarditis resulting
from septicemia has been observed historically. The diagnosis is confirmed with
bacterial cultures or urine DNA testing. If denudation of the epithelium in the
urethra or vas deferens occurs from treatment, urethral strictures and
infertility due to reproductive tract obstruction may develop. Risk factors for
contracting the infection include having multiple sexual partners, a partner
with a past history of any sexually transmitted diseases, and unprotected sex.
Antibiotics are curative. The term nongonorrheal urethritis or nonspecific
urethritis refers to urethritis due to sexually transmitted diseases other than
gonorrhea. This form of urethritis is more common than gonorrheal urethritis,
with approximately 89 million new cases diagnosed annually worldwide versus 62
million new cases of gonorrhea. The clinical presentation can be identical to
that of gonorrhea and concurrent infections with several different organisms
can occur. Responsible organisms are most commonly Chlamydia trachomatis,
the mycoplasma species Ureaplasma urealyticum and Mycoplasma
genitalium, and herpes simplex type II virus. Nonspecific urethritis, when
associated with conjunctivitis and arthritis, is referred to as Reiter syndrome and may
be a consequence of sexually transmitted infections by nongonorrheal organisms.
Urethral strictures can present with urethritis-like symptoms, and in rare
instances the underlying cause may be a papilloma, polyp, or cyst of the
urethra. Bacterial nongonorrheal urethritis is routinely cured with antibiotics.
Trichomonas
vaginalis is a sexually transmitted, microscopic parasite that causes
trichomoniasis. This is a relatively
common form of nongonorrheal urethritis with an estimated 8 million new cases
annually in the United States. Trichomonads are usually found in the urethral
exudate or urethral urine and are recognized microscopically by their active
motility and propelling flagella. Patients may be asymptomatic or have a slight
thin, milky white urethral discharge in the morning. Itching, dysuria, and possibly
urinary urgency may be present.
It is curable with antibiotics.