RADIAL LONGITUDINAL DEFICIENCY
 |
| Forearm Manifestations of Radial Longitudinal Defeciency |
The cause of
radial longitudinal deficiency remains unknown. Several factors have been
proposed as potential insults to the developing limb, including intrauterine
compression, vascular insufficiency, environmental insults, maternal drug
exposure, and genetic mutations. Upper limb development occurs during the first
4 to 7 weeks of embryonic life and coincides with the appearance of the
cardiac, renal, and hematopoietic systems. Thus, single or multiple embryonic
insults can result in malformations of several organ systems. Therefore, all
children presenting with a radial-sided dysplasia, regardless of severity,
mandate thorough evaluation for associated medical conditions. Of primary
concern are the cardiac, renal, gastrointestinal, and hematopoietic systems.
The spectrum of these malformations ranges from mild to devastating.
ANATOMIC
MANIFESTATIONS AND CLASSIFICATIONS
Thumb
The length
of the average thumb extends to the distal half of the index finger’s proximal
phalanx in adduction, reaching the palmar surface of the small finger’s
proximal phalanx in opposition. Absence of thumb function, either from
congenital or traumatic afflictions, has been estimated to diminish overall
hand function by 40%.
Blauth
classified thumb hypoplasia into five types according to thumb size, depth of
the first web space, intrinsic muscle deficiency, extrinsic muscle deficiency,
and bony/ligamentous joint stability. Manske and col-leagues divided type III
thumb hypoplasia into subtypes IIIA and IIIB, based on the presence or absence
of a stable first carpometacarpal joint. This subdivision has critical
implications to surgical management and separates the reconstructible thumb
(IIIA) from the largely nonreconstructible thumb (IIIB).
Forearm
The forearm
in radial dysplasia has a deficient skeleton, hypoplastic or absent
musculature, and altered neurovascular anatomy. Forearm length and radial
deviation of the hand/carpus are
directly related to the severity of radial deficiency. The relative shortening
of the limb remains constant throughout growth.
Bayne and
Klug classified radial dysplasia into four types based on the radiographic
severity of skeletal deficiency. Type IV dysplasia is the most prevalent,
defined by complete absence of the radius. The ulna is bowed with marked radial
and palmar displacement of the hand. The forearm in Type IV dysplasia averages 60% of the length of the
contralateral normal side.
TREATMENT
The overall
health of the child and the severity of the osseous and soft tissue deformities
guide long-term treatment plans. Parents and families are instructed on realistic goals for
improving function and cosmesis of the upper limb.
Nonoperative
management is the definitive treatment for children with minimal deformity and
stable joints as well as in children with severe deformity and/ or associated
anomalies precluding safe surgical intervention. Absolute contraindications to
operative reconstruction include (1) adults and older children with established
patterns of functional compensation, (2) mild deformities with good function
and cosmesis, (3) associated medical anomalies precluding safe operative
reconstruction, and/or (4) severe, bilateral elbow extension contractures that
rely on wrist flexion and radial deviation for placement of the hand to the
face.
The goals
for operative reconstruction are to optimize upper limb length, straighten the
forearm axis, and either reconstruct or ablate the thumb and pollicize the
index finger. The forearm and thumb are addressed in staged procedures. The
initial surgery is undertaken at 6 to 12 months of age and involves realigning
and stabilizing the hand/carpus on the distal ulna. Thumb
reconstruction/ablation begins 6 months after wrist realignment with the
overall goal of completing all reconstructions by 18 months of age, thus
allowing the child to achieve usual developmental milestones.
Forearm
Current
techniques attempt to achieve and maintain deformity correction and stability
while optimizing growth, improving digital and wrist range of motion and
enhancing function. Maintaining the bony carpus and distal ulnar physis are
critical to optimizing upper limb length, wrist motion, and future growth
potential, which are prerequisites for a successful surgical outcome. Recently,
soft tissue distraction devices have been utilized as a staged procedure to
achieve passive reduction of the hand/carpus in recalcitrant cases.
Thumb
Anatomic
reconstruction is appropriate in children demonstrating functional
incorporation of their thumbs. The objective is to obtain a stable digit for
pinch, grip, and prehension. Reconstruction has the advantages of maintaining a
five-digit hand with the potential for polyaxial rotation at the thumb’s
basilar joint surgical impossibilities
with ablation and index finger pollicization.
Children
with Blauth types IIIB, IV, and V have poor cerebrocortical representation of
their thumbs. Reconstruction may improve cosmesis but will not restore
functional use of an ignored digit. With time, the functionally excluded thumb
will become a liability. The surgical details of ablation and index finger
pollicization have been well documented. The goals of pollicization are to (1)
preserve the neurovascular anatomy, (2) shorten the index metacarpal via
diaphyseal deletion, (3) rotate
and stabilize the index finger (in 120 degrees pronation, 40 degrees abduction, and 15 degrees extension), and (4)
reattach and balance the musculotendinous units.
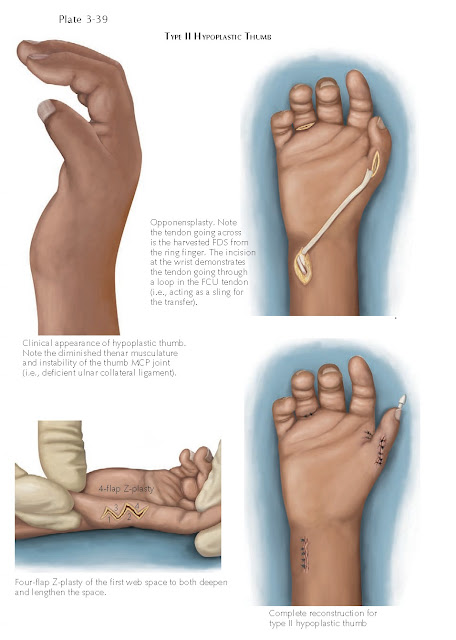 |
| Type II Hypopastic Thumb |
SUMMARY
Management
of radial longitudinal deficiency challenges even the most experienced
orthopaedic surgeon. Cooperative effort between the orthopaedist, pediatrician,
geneticist, and medical specialists ensures optimal medical evaluation and
treatment of these children.
Surgical
reconstruction aims to realign and stabilize the forearm, wrist, and hand while
providing a functional thumb for strong pinch and grasp. Current and future
research strives to identify the underlying developmental insults responsible
for deformity and to enhance operative management to optimize forearm length,
minimize recurrence, improve both wrist stability and motion, and further
advance thumb reconstruction/ablation-pollicization.




