LARYNGEAL AND TRACHEAL STENOSIS
The unique anatomy and
delicate tissues of the larynx and trachea predispose these sites to scarring
and stenosis in response to injury. Some of the more common causes include
prolonged endotracheal intubation, long-term tracheostomy, bacterial or viral
infection, systemic inflammatory conditions, neoplasia, and trauma. In many
cases, the stenosis is a relatively late sequela of the initial pathologic
process and may not be recognized until it progresses to the point of
symptomatic airway compromise (stridor or dyspnea) or impaired laryngeal
function (hoarseness).
Laryngeal
stenosis may occur at any level within the larynx. Supraglottic and glottic
stenosis are usually a result of external trauma or prolonged intubation but
are also seen with caustic ingestions, inhalation burns, and postsurgical
scarring. Subglottic stenosis is the most common form of laryngeal stenosis.
Prolonged endotracheal intubation can damage the thin inner perichondrium of
the cricoid cartilage, leading to circumferential scarring and cicatrix
formation. Long- term tracheostomy tubes can also cause subglottic stenosis as
a result of superior migration of the tube and ensuing destruction of the
cricoid ring. Other common causes of subglottic stenosis include
laryngopharyngeal reflux, Wegener granulomatosis, and a congenital form seen in
young children. When a specific cause cannot be identified, the term idiopathic
subglottic stenosis (ISS) is used. It is likely that many cases of ISS are
caused, at least in part, by unrecognized laryngopharyngeal reflux or autoimmune
disorders.
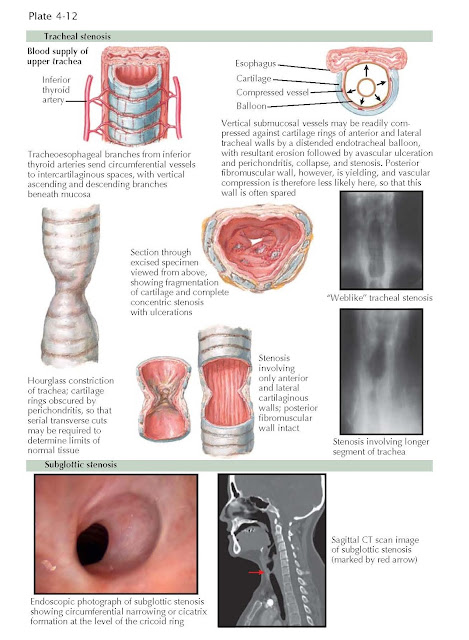
Tracheal
stenosis is a potentially devastating sequelae of prolonged endotracheal
intubation and tracheostomy in patients with respiratory failure requiring
cuffed tubes for mechanical ventilation. In the anterior and lateral tracheal
walls, the vertical blood vessels that course between the mucosa and the
cartilage rings may be readily compressed by a distending cuff or balloon.
Decreased blood supply leads to perichondritis, avascular necrosis, and
fragmentation of the tracheal cartilage. The resultant stricture often has a
triangular configuration on transverse section because of anterior weakening of
the cartilaginous arch with lateral wall collapse. Posteriorly, the membranous
trachea is more pliable, and the vascular supply is less likely to be
compressed. Thus, in about 50% of cases of postintubation or post- tracheostomy
balloon stenosis, the posterior tracheal wall is spared.
The
characteristics and extent of tracheal stenosis can be demonstrated
radiographically with traditional tomography in the frontal and lateral
projections or with computed tomography (CT) images in the coronal and sagittal
planes. The stenotic segment may be narrow and weblike, involving only one
tracheal ring, or it may be longer, involving two to five tracheal rings with
tapering margins. If the affected segment is thin or pliable, obstruction may
only occur with inspiration or expiration (tracheomalacia), depending on
whether the affected segment is extrathoracic (neck) or intrathoracic (thorax),
respectively. Tracheomalacia may result in greater functional impairment than
is apparent radiographically. If dynamic collapse is suspected, flow- volume loops
demonstrating reduced inspiratory or expiratory flow or fiberoptic bronchoscopy
demonstrating inspiratory or expiratory collapse may be useful diagnostic
tools. In some cases, multiple stenoses may occur, especially after the use of
tubes of different lengths or tubes with double cuffs.
Postintubation
and posttracheostomy balloon steno- sis remains a serious problem despite the
advent of low-pressure cuffs and increased vigilance in the clinical care
setting. It has been recommended that the cuff be deflated at intervals to avoid
an excessively prolonged compression of the tracheal mucosa. The problem with this method
is that the cuff may not empty completely, and if it is reinflated with the
minimal fixed volume of air recommended for filling, overinflation may occur.
Proper cuff pressures are best achieved by inflating under auscultatory control
until there is no leakage of air with positive-pressure ventilation. If
stenosis develops despite these measures, surgery in the form of endoscopic
laser incision and dilatation or tracheal resection with anastomosis may be necessary.