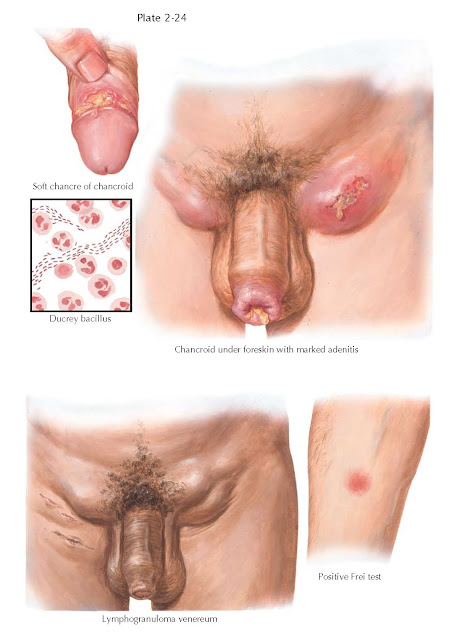
CHANCROID, LYMPHOGRANULOMA VENEREUM
Chancroid, formerly “soft chancre,” is a
sexually transmitted disease characterized by painful ulcers, and painful
inguinal lymphadenopathy (buboes). The causative organism, Haemophilus
ducreyi, was found by Ducrey in 1889. It is a gram-negative
coccoid-bacillary rod that is found at the bottom of the initial ulcer, from
which it spreads through lymphatic channels to the inguinal nodes, causing
necrosis. H. ducreyi enters the skin through an epithelial break,
usually following sexual intercourse. With a mean incubation period of 5 to 7
days, the bacteria secrete a cytolethal toxin that inhibits cell proliferation
and induces cell death, causing the characteristic ulcer formation.
The ulcer,
very painful and often located around the sulcus of the glans, is characterized
by a “soft chancre” with steep edges, irregular borders, undermined skin, and a
ring of erythema. It begins as a small congested area that develops into a
macule and later a pustule surrounded by a hyperemic zone. A dirty floor due to
the presence of exudate and sloughing tissue, and a profuse, purulent discharge
are typical. Inguinal buboes may rupture after becoming an abscess and heal
with scarring. This can result in chronic lymphatic obstruction and late
elephantiasis-like changes to the penile and scrotal skin. The diagnosis is
made from the clinical appearance of the lesions, by polymerase chain reaction
(PCR) directed against one of two genomic segments (ribosomal RNA gene or the GroEL
gene), or by Gram stain showing H. ducreyi appearing like “schools
of fish,” “railroad tracks,” or “fingerprints.” Organism culture is unreliable
and insensitive. Immunochromatography is a more rapid but less available test
that uses monoclonal antibodies to the hemoglobin receptor on the bacteria.
Treatment involves incision and drainage of buboes and curative antibiotics.
Lymphogranuloma
venereum (LGV) is a sexually transmitted disease caused by invasive Chlamydia
trachomatis. LGV may begin as a self-limited, painless genital ulcer that
occurs at the contact site 3 to 12 days after inoculation. It usually heals
rapidly, unless secondary infection
occurs. The secondary stage occurs from 10 to 30 days later as the infection
spreads to inguinal lymph nodes. Systemic signs of fever, decreased appetite,
and malaise may occur as well. Buboes are typically painful at first and are
associated with necrosis and abscess formation with chronic infection. There
can be varying degrees of lymphatic obstruction and chronic edema caused by
fibrosis as a result. The diagnosis is made by the appearance of the chronic
ulcerative process in the inguinal area, and historically (before 1974) by a positive
skin test (Frei test) following intra- dermal injection of Chlamydia antigen.
Ulcer biopsy histology is not pathognomonic. Complement fixation is more
sensitive (80%) but it has cross-reactivity with other Chlamydia species.
Other blood tests such as microimmunofluorescence test for the L-type serovar of
C. trachomatis and PCR are very sensitive and specific, but test
availability is limited. Bacterial culture from aspirated material is definitive
bu lacks sensitivity. Treatment
with antibiotics is curative.