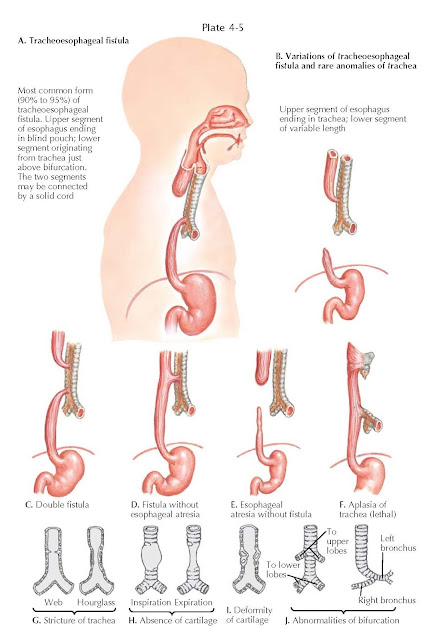
Tracheoesophageal
Fistulas and Tracheal Anomalies
Tracheoesophageal fistula (TOF) and esophageal atresia rarely occur as
separate entities, but they are often seen in various combinations: esophageal
atresia with upper fistula, lower fistula, and double fistulas. Approximately 10%
of infants with esophageal atresia do not have a fistula, but there is a long
gap between the esophageal segments. An isolated tracheoesophageal fistula (H or
N fistula) can occur without an esophageal atresia. The cause of these
congenital anomalies is not well understood. Esophageal atresia is usually
sporadic and rarely familial.
Maternal polyhydramnios and a small
or absent fetal stomach bubble on antenatal ultrasonography suggest the
possibility of esophageal atresia antenatally. Postnatally, the diagnosis can
be suspected in a newborn infant who has excessive mucus and cannot handle his
or her secretions adequately. Suction provides temporary relief, but the
secretions continue to accumulate and overflow, resulting in aspiration and respiratory
distress. Feeds are also regurgitated and aspirated. The TOF provides a
low-resistance pathway for respiratory gases and gastric distension, and
subsequent rupture may further compromise ventilation.
Formerly, the diagnosis was made by
using a contrast study with barium or Gastrografin (meglumine diatrizoate);
however, there is the danger of aspirating these materials into the lungs. The
diagnosis can readily be made by passing a fairly large radiopaque plastic catheter
through the nose or mouth into the pouch. When the catheter cannot be advanced
into the stomach, the catheter should then be taped in place and put on constant
gentle suction. This keeps the pouch free of saliva and minimizes the chances
of aspiration pneumonitis. On the chest radiograph, it will be noted that the
tip of the catheter is usually opposite T2-T3. If the surgeon prefers a
contrast study, no more than 0.5 mL of contrast material should be introduced
through the catheter, with the child in the upright position. Radiography will
show the typical esophageal obstruction, and the contrast material should then
be immediately aspirated.
Initial management is aimed at
keeping the airway free of secretions using a 10-Fr double lumen Replogle tube
in the proximal pouch on continuous low pressure suction. The ideal surgical
procedure consists of disruption of the fistula and an end-to-end anastomosis of
the esophagus. If there is a long gap between the esophageal segments, surgery
is delayed to allow the pouches to elongate and hypertrophy over a period of up
to 3 months. During this time, the infant is fed through a gastrostomy, and the
upper pouch is kept clear of secretions.
Anomalies and Strictures of The Trachea
Tracheal anomalies are very rare.
With stricture of the trachea, there is local obstruction of the passage of
air. In the absence of cartilage, the trachea can collapse and therefore
obstruct on expiration. With deformity of cartilage, there is obstruction on
inspiration and expiration. When abnormal bifurcations are
present, the right upper or left upper lobe bronchi (or both) arise
independently from the trachea.
Clinically, stenosis may be
localized or diffuse. The localized form is caused by a web of the respiratory
mucosa or by excessive growth of tracheal cartilage. The diffuse form is caused
by a congenital absence of elastic fibrous tissue between the cartilage and its
rings in the trachea or by an absence of cartilage. Clinically, obstruction
of the trachea causes chronic dyspnea; cyanosis, especially on exercise; and
repeated attacks of respiratory tract infection. The diagnosis is established
by bronchoscopy and by radiography.
For localized obstruction, surgery
is advisable, either dilatation or excision with end-to-end anastomosis.
Resection and anastomosis of the trachea can be carried out, including up to
six tracheal rings. For generalized stenosis, only supportive therapy is available.