GRANULOMA ANNULARE
Granuloma
annulare is a commonly encountered rash. The etiology of this rash is unknown.
There are various clinical presentations, including localized, generalized,
subcutaneous, actinic, and perforating forms. The generalized version has been
seen in association with diabetes. Most cases spontaneously resolve. Multiple
treatment strategies exist.
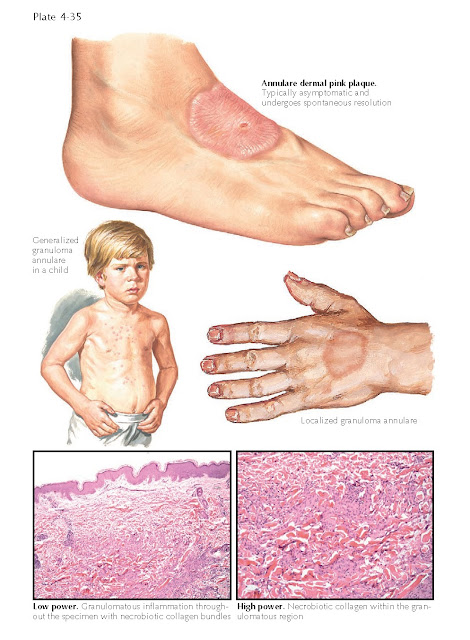
Clinical Findings: Granuloma annulare is a rash that occurs
commonly in children but can be seen in any age group. There is no race
predilection, but it is twice as common in females as in males. The localized
form of granuloma annulare typically starts insidiously as a small,
flesh-colored to slightly yellow papule that expands centrifugally. Once the
lesion gets to a certain size, its characteristic appearance becomes evident.
Fully formed, the area appears as an annular plaque with minimal to no surface
change. The plaque appears to have a raised rim around the edge, and the
central portion of the lesion is almost normal in appearance. The peripheral
rim is slightly yellow in color. The lesions can be entirely flesh colored.
Patients experience minimal symptoms. Slight itching may be present. It is not
uncommon to have multiple areas of involvement. The dorsal aspects of the feet
and hands are common locations for this rash. Some patients relate that their
rash is improved during the summer months. The lesions can range from small
papules a few millimeters in diameter to larger plaques a few centimeters in
diameter. If only small papules exist, a biopsy is required for diagnosis. The
clinical appearance of the larger plaques is so characteristic that the
diagnosis can be made clinically.
The generalized version of
granuloma annulare consists of numerous widespread papules and small plaques.
In most cases, there are no annulare-appearing plaques; the diagnosis is considered
clinically, but a biopsy is required to confirm the diagnosis. This form occurs
almost exclusively in adults and may be seen in association with diabetes.
Patients with a diagnosis of generalized granuloma annulare should be screened
for diabetes. The other variants of granuloma annulare are uncommonly
encountered. They include the subcutaneous form, the perforating variant, and
the actinic variant. The actinic variant may be considered a unique entity,
termed annular elastolytic giant cell granuloma. Subcutaneous granuloma
annulare manifests as deep- seated nodules within the dermis. A diagnosis is
made via biopsy. This variant appears to be more common in children. The
perforating variant is the rarest form and is the only variant to exhibit surface
change. The areas of involvement develop small erosions. This is reported to
occur most commonly on the dorsal surface of the hands.
Pathogenesis: The etiology is unknown. It has been theorized
to represent an abnormal immune response to a foreign antigen such as a virus
or bacteria. This has not been proven, and many other theories of
pathogenesis exist. Ultimately, the collagen within the lesions is disrupted,
and the resulting inflammatory response causes the clinical findings.
Histology: The histological findings in biopsy specimens
of granuloma annulare are very specific. There are areas of necrobiotic
collagen with a surrounding granulomatous infiltrate. The collagen is being
destroyed centrally. A varying amount of mucin is present. The main histological
differential diagnosis is between granuloma annulare and necrobiosis lipoidica.
The inflammation in necrobiosis lipoidica is typically oriented
across the entire biopsy specimen in a layered fashion. Histological variants
of granuloma annulare exist, including interstitial granuloma annulare.
Treatment: Localized forms of granuloma annulare that are
asymptomatic and not causing any distress to the patient can be left alone.
Most cases resolve spontaneously over time with no residual scarring and no clinically
noticeable abnormality. Topical corticosteroids may be used to try to decrease
the inflammatory response. Intralesional corticosteroids can be
used in some cases, but the risk of atrophy from the steroid injection must be
considered. Generalized forms are not amenable to topical therapy. Phototherapy
has been used successfully. Psoralen + ultraviolet A light (PUVA) therapy has
had more success than ultraviolet B (UVB) light therapy, most likely because
UVA light penetrates deeper into the dermis than UVB. Phototherapy with UVA1
appears promising.