GRAFT-VERSUS-HOST
DISEASE
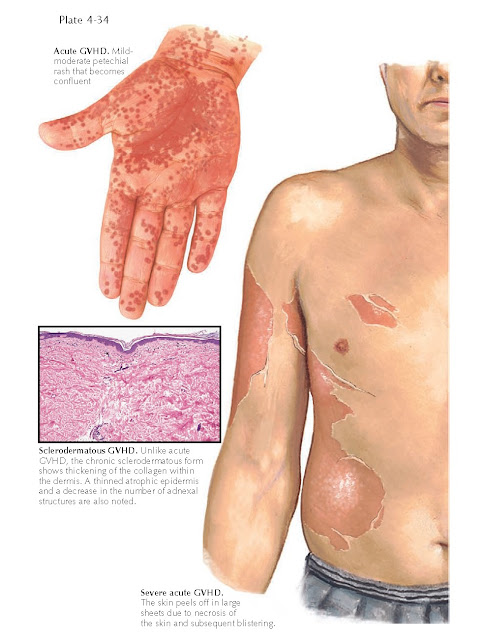
With the ever-increasing number of bone marrow transplantations and
increasing survival rates of patients undergoing these procedures,
graft-versus-host disease (GVHD) is becoming more prevalent. Two distinct
clinical cutaneous forms exist, acute and chronic, each with its own
manifestations and treatment options. Acute GVHD is often manifested by
mucocutaneous eruptions that can range from a mild macular rash to
life-threatening blistering of the skin. Chronic cutaneous GVHD is entirely
different in clinical manifestation than its acute counterpart. The two forms
are also seen during specific time frames: Acute GVHD is most likely to occur
within the first 3 months after transplantation, whereas chronic GVHD occurs
later, typically 4 months or longer after transplantation.
GVHD can be seen not only after
bone marrow transplantation but in any immunosuppressed patient who has
receives antigenically and immunologically viable cells from a donor. This may
occur during organ transplantation or, rarely, during blood transfusion. The
use of leuko-poor blood has helped decrease the chance of GVHD after blood
transfusions.
Clinical Findings: Acute GVHD is a common complication after bone
marrow transplantation. The incidence has been reported to be as high as 90%.
The degree of involvement is variable. GVHD affects males and females equally,
and there is no racial preference. Patients who develop acute GVHD typically
begin having symptoms soon after their cell counts recover, usually 1 to 2
weeks after transplantation. Skin rashes that develop within the first week
after transplantation are usually not from GVHD. The skin, upper and lower
digestive tract, and liver are frequently involved, and these organ systems are
evaluated to help make the diagnosis of GVHD. The rash of acute GVHD can range
from a fine maculopapular rash to severe blistering of the skin that can
resemble toxic epidermal necrolysis and can be life-threatening. It is
difficult, if not impossible, to predict the development and course of acute
GVHD. These patients are always taking multiple medications, and the
differential diagnosis includes a drug rash. Histological evaluation of a skin
biopsy cannot differentiate the two. The coexistence of mucositis, diarrhea,
and elevated liver enzymes makes the diagnosis of acute GVHD more plausible.
The constellation of all these symptoms leads one to make the diagnosis.
Chronic GVHD has entirely different
clinical manifestations. This form of GVHD typically begins 3 to 6 months after
transplantation. The skin is the organ system most commonly involved. Two
distinct forms of chronic cutaneous GVHD occur, lichenoid and sclerodermatous.
The lichenoid variant manifests as red papules, patches, and plaques. They can
occur anywhere on the surface of the skin. There is a slight resemblance to
lichen planus. The sclerodermatous variant is less common and manifests as
thickened, firm skin with poikilodermatous changes. The surface of the skin is
shiny, and the loss of adnexal structures is variable. This variant of chronic
GVHD can be localized to a small area, or it can be generalized and may include
the entire surface area of the skin. The amount of surface area involved is
directly related to the morbidity the patient experiences.
Histology: Histological evaluation of skin biopsy
specimens cannot differentiate acute GVHD from drug exanthems. Acute GVHD has
been graded on a histological scale of 1 to 4. Grade 1 shows basal layer vacuolar
and interface changes; grade 2 shows signs of keratinocyte death; grade 3 shows
clefting within the subepidermal space; and grade 4 is full bulla formation
with epidermal parting.
Lichenoid chronic GVHD shows a
lichenoid dermatitis with a predominantly lymphocytic infiltrate. The
sclerodermatous form of chronic GVHD shows abnormally thick dermal collagen,
much like that seen in scleroderma.
Treatment: The treatment of acute GVHD is based on the
clinical symptoms and the type of skin lesions.
Corticosteroids are commonly used
in cases of GVHD, both acute and chronic. The acute form has also been treated
with FK506 and cyclosporine. Many other immunosuppressants have been used.
Chronic GVHD is difficult to
manage. There is no cure for GVHD, and treatment is directed at stabilizing and
improving skin function and increasing the patient’s functional capabilities.
Phototherapy has been use successfully, as has extracorporeal photopheresis.