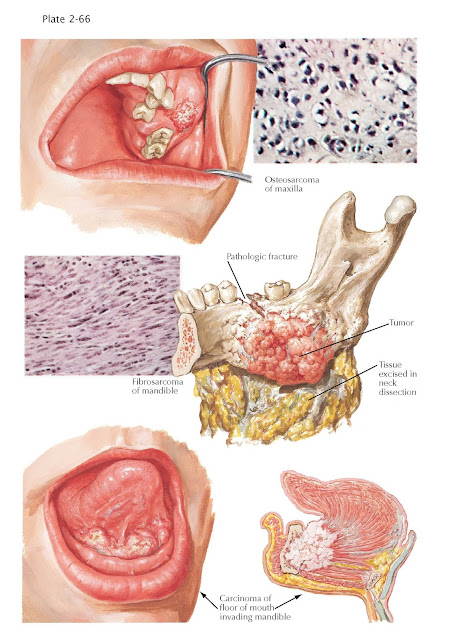
Malignant
Tumors of Jaw
Malignant tumors involving the jawbones are nearly always epidermoid
carcinomas, which are formed from peripheral epithelium and invade the bones
secondarily. Malignant transformation of a benign neoplasm, particularly of a
mixed tumor of salivary tissue, is sometimes seen. Metastases of primary
carcinoma of the thyroid, breast, or prostate to the jaws via the blood-stream
are very rare, and so are malignant primary tumors of odontogenic, osteogenic,
or other origin.
Though osteogenic sarcoma is
the most common and most malignant of bone tumors, only 2% to 3% of cases
appear in the jawbones. Trauma is believed to play a role in its etiology, as
evidenced by clinical histories and experimental production in animals.
It is a solitary growth, which differentiates it from
various tumors of nonosteogenic origin (e.g., endothelioma, multiple myeloma).
The maxillary tumor illustrated has caused wide, mottled destruction of bone,
as revealed by radiographic findings. The classic “sun-ray” pattern seen in the
long bones is seldom appreciated in the jaws, although new bone formation may
be noted. The swelling can involve the entire maxilla and portions of the
palate, with invasion into the antrum. Pain, paresthesia, swelling, tenderness,
and displacement of teeth, with disturbed mastication, are associated symptoms.
Hematologic metastasis can be an early phenomenon.
The histopathologic picture
shows immature cells, which are pleomorphic and hyperchromatic, with some
admixture of stroma, myxomatous tissue, cartilage, and osteoid tissue.
Pathologic descriptions sometimes refer to osteolytic, osteoblastic, and
telangiectatic (vascular) types. The osteoblastic variety tends to grow more
slowly than the vascular type.
Fibrosarcoma may be formed peripherally and invade the
jaws, or centrally from tissues of the tooth, germ or other mesenchymal
enclaves, or connective tissue elements of the nerves and blood vessels. In the
case of rapidly advancing osteolytic lesions, clinical recognition is usually
delayed until loosening of the teeth, encroachment on the antrum or nose, or
perforation of the cortical plate has occurred. No evidence of periosteal
activity is noted, as is sometimes the case with osteosarcoma. Frequently,
proud flesh in the socket of an extracted tooth is the first sign of an
underlying malignancy. In the mandibular tumor chosen for illustration,
pathologic fracture was caused by the widespread destruction of medullary bone.
The tumor mass has perforated the lingual wall of the mandible, with invasion
of soft tissues in the floor of the mouth and neck. Radiographic examination
showed a blurred, diffuse osteolytic area, denoting an invasive rather than an
expansile growth. The microscopic picture reveals spindle-shaped cells, with
anaplasia and varying amounts of intercellular collagenous tissue; in the
rapidly growing forms, a plump cellular shape with frequent mitoses is seen,
but little intercellular material is present.
Carcinoma invading the
mandible is illustrated
in a lesion of the anterior floor of the mouth. The tumor here is a
grade III malignancy, causing early infiltration of cortical bone, with
progress along the haversian canals and destruction of a large portion of
cancellous bone. At the same time, extension occurs through the lymph
channels to involve the submandibular
and cervical nodes, as well as the soft tissues contiguous to the tumor. The
base of the tongue has become fixed and immobile. A fungating tumor mass is
observed in the floor of the mouth, which is secondarily infected and extremely
painful, with a foul exudate and odor.