ALLERGIC CONTACT DERMATITIS
Allergic contact dermatitis is one of the rashes most frequently
encountered in the clinician’s office. It is responsible for a large proportion
of occupationally induced skin disease. Urushiol from the sap of poison ivy,
oak, or sumac plants is the most common cause of allergic contact dermatitis in
the United States. The clinical morphology, the distribution of the rash, and
results from skin patch testing are used to make the diagnosis. Patch testing
is performed when the causative agent is unknown. Nickel has been the most
frequent cause of positive patch testing in the world for years. Urushiol is
not tested clinically, because almost 100% of the population reacts to this
chemical.
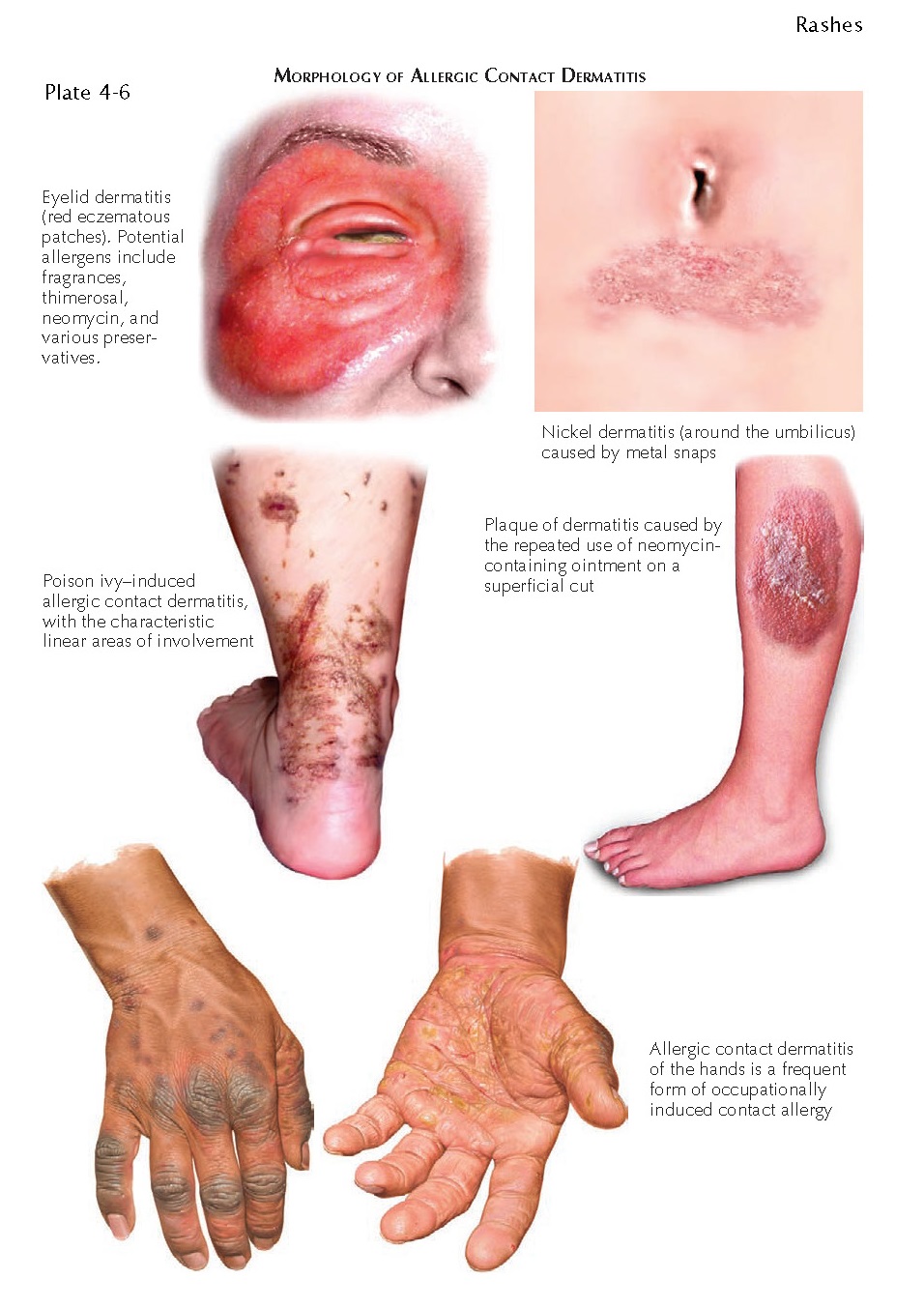 |
| MORPHOLOGY OF ALLERGIC CONTACT DERMATITIS |
Clinical Findings: Allergic
contact dermatitis can manifest in a multitude of ways. The acute form may show
linear streaks of juicy papules and vesicles. Variable amounts of surrounding
edema can be seen. Edema is much more common in the loose skin around the
eyelids and facial region. Chronic allergic contact dermatitis can manifest
with red-pink patches and plaques with various amounts of lichenification.
There are localized forms and generalized forms. One of the unique forms of
allergic contact dermatitis is the scattered generalized form. Pruritus is an
almost universal finding, and it can be so severe as to cause excoriations and
small ulcerations.
The prototype of allergic contact
dermatitis is the reaction to the poison ivy family of plants. After contact
with this plant, urushiol resin is absorbed into the skin and initiates the
immune system response to cause allergic contact dermatitis. The dose and the
duration of contact with the allergen are important influences on the severity
of the rash that develops. Between 3 and 14 days after exposure, the patient
notices linear juicy papules and vesicles forming at the sites of contact. The
most commonly affected areas are the extremities. Air-borne contact dermatitis
may be seen from burning of wood with the poison ivy vine present. These
reactions are usually seen on skin that was not covered with clothing, and they
can be very severe on the face and eyelids, often causing massive swelling and
impeding vision.
The location of the dermatitis
can be used as a clue to the diagnosis. A nurse with hand dermatitis may be
allergic to a component of the gloves being worn occupationally. A young child
with a lichenified rash around the umbilicus may be allergic to a metal
component of a pant snap or zipper. The most common culprit in these cases is
nickel. Finger dermatitis may be caused by the application of acrylic nails or
nail polish. Allergic contact dermatitis can also be seen within the oral
cavity, most commonly adjacent to dental amalgams or prostheses. Oral allergic
contact dermatitis can mimic oral lichen planus. Lichen planus is usually
widespread and affects the mucosa and gingiva both adjacent to and distant from
any dental restorations.
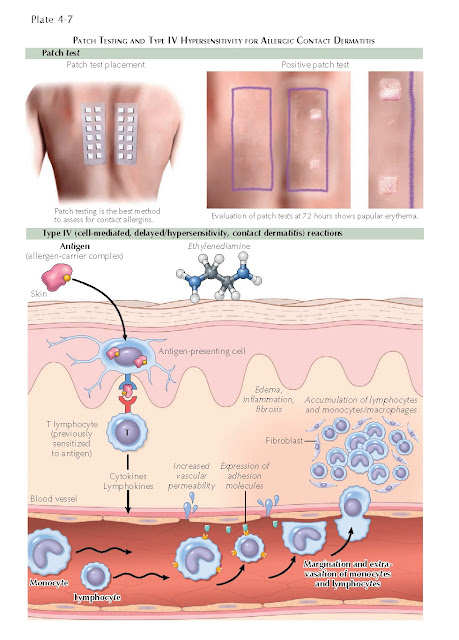
The diagnosis in all these cases
can be made based on patch testing. Chambers loaded with specific
concentrations and amounts of known allergens are applied to the back of the
individual. The patches are left on for 48 hours and then removed. After an
hour, the first reading is made, based on the reaction seen under the chamber.
Elevation of the skin or vesiculation is considered to be a positive reaction.
The presence of only macular
erythema needs to be interpreted cautiously but can be considered a positive
result in certain situations. Pustular reactions are considered to be irritant
reactions and not relevant. The patient must come back for a final reading 3 to
7 days after application of the patches. This is the most critical reading and
gives the most valuable information.
Pathogenesis: Much
is known about the mechanism of allergic contact dermatitis. This form of
dermatitis requires a sensitization and elicitation phase for development.
During the sensitization phase, the patient is exposed for the first time to
the antigen. The antigen is absorbed through the skin and is phagocytosed by an
antigen-presenting cell within the epidermis. The antigen-presenting cell internalizes
the antigen and processes it within its lysosomal apparatus. The processed
antigen is then sent to the cell surface and expressed on a human leukocyte
antigen (HLA) molecule. The antigen-presenting cell migrates to the local
draining lymph node and presents the antigen in association with the HLA
molecule to T cells. The T cells recognize each individual antigen and
proliferate locally, resulting in a clone of lymphocytes that recognize that
specific antigen; these lymphocytes then remain ready for when the patient
comes in contact with the same antigen in the future.
During the elicitation phase, the
patient is reexposed to the antigen. The antigen-presenting cells again process
the antigen and present it to the newly cloned lymphocytes, which migrate back
to the skin and cause the clinical findings of edema, spongiosis, vesicles, and
bullae. If the antigen is exposed in a chronic manner, the findings will be
less acute in nature, and the typical findings of a chronic dermatitis are
seen.
This entire process is dependent
on the size and permeability of the antigen, the recognition and processing of
the antigen by the antigen-presenting cell, and the complex interactions among
multiple T and B cells. Antign-presenting cells and B cells are required for
activation of the T cells and propagation of the allergic contact dermatitis.
Histology: The
initial finding in acute allergic contact dermatitis is spongiosis of the
epidermis with an associated superficial and deep lymphocytic infiltrate with
scattered eosinophils. As the rash progresses, the spongiosis can worsen, and
intraepidermal vesicles start to form. The vesicles may eventually coalesce
into large bullae.
Chronic allergic dermatitis
usually shows acanthosis with spongiosis and eosinophils within the infiltrate.
A superficial and deep perivascular lymphocytic infiltrate is seen.
Excoriations can also be appreciated.
 |
| PATCH TESTING AND TYPE IV HYPERSENSITIVITY FOR ALLERGIC CONTACT DERMATITIS |
Treatment: Acute
localized allergic contact dermatitis can be treated with a potent topical
steroid and strict avoidance of the offending agent. Oral sedating
antihistamines work better for the pruritus than their non-sedating
counterparts do. Soaks that help to dry the dermatitis are helpful and include
aluminum acetate (Domeboro’s solution). Because the most common culprit is the
poison ivy plant, time should be taken to explain to the patient the appearance
and nature of this plant. As a good rule of thumb, if a plant has three leaves,
it could be poison ivy: “Leaves of three, let it be.” Allergic contact
dermatitis that is widespread or that affects the eyelids, hands, or groin
region can be treated with a tapering dose of oral corticosteroid over a 2- to
3-week period. If the steroid is tapered too quickly, the patient may
experience a poststeroid flare of their dermatitis, which can be resistant to
further corticosteroid therapy.
Patients who do not respond to
these measures should undergo patch testing to determine whether another
antigen is causing or provoking the dermatitis. Without the use of patch
testing, the allergen will remain unknown and the dermatitis will persist. Not
infrequently, patients are found to be allergic to a fragrance or preservative
that is an ingredient in one of their personal care products. Once they stop
using the product, the dermatitis finally resolves.




