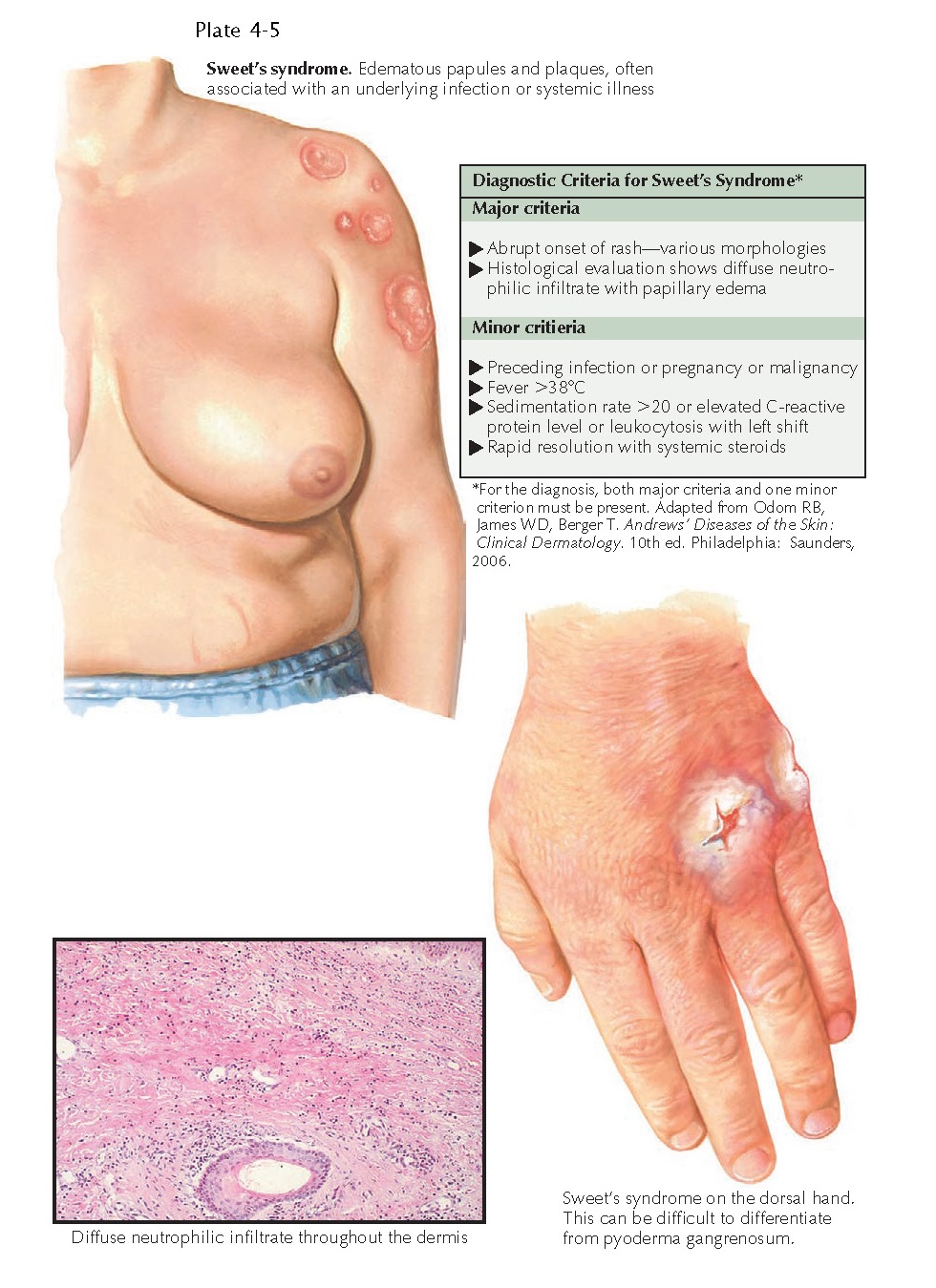
ACUTE FEBRILE NEUTROPHILIC DERMATOSIS
(SWEET’S SYNDROME)
Acute febrile
neutrophilic dermatosis is an uncommon rash that most often is secondary to an
underlying infection or malignancy. The diagnosis is made by fulfilling a
constellation of criteria. Both clinical findings and pathology results are
required to make the diagnosis in a patient with a consistent history.
Clinical Findings: Acute febrile neutrophilic dermatosis is
often associated with a preceding infection. The infection can be located
anywhere but most commonly is in the upper respiratory system. Females appear
to be more likely to be afflicted, and there is no race predilection. Patients
present with fever and the rapid onset of juicy papules and plaques. Because
the papules can look as if they are fluid filled, they are given the
descriptive term juicy papules. They can occur anywhere on the body and
can be mistaken for a varicella infection. Patients also have neutrophilia and
possibly arthritis and arthralgias. If this condition is associated with a
preceding infection, it is usually self-limited and heals without scarring,
unless the papules and plaques are excoriated or ulcerated by scratching.
Variable amounts of pruritus and pain are associated with this skin disease. When
one is evaluating a patient with this condition, a thorough history is
required. A skin biopsy must be performed. A chest radiograph, throat culture,
and urinalysis should be performed to assess for the possibility of bacterial
infection.
Lymphoproliferative malignancies
have also been seen in association with Sweet’s syndrome. The malignancy often
precedes the rash, and the skin disease is believed to be a reaction to the
underlying malignancy. It is important to obtain specimens from these patients
for histological evaluation and culture for aerobic, anaerobic, mycobacterial,
and fungal organisms. The main differential diagnosis is between an infection
and Sweet’s syndrome in cases associated with a malignancy. The most common
malignancy associated with acute febrile neutrophilic dermatosis is acute
myelogenous leukemia. The prognosis in these cases is directly related to the
underlying malignancy. Often, the skin disease continues to recur unless the
malignancy is put into remission.
A few medications have also been
shown to induce Sweet’s syndrome, including granulocyte colonystimulating
factor (G-CSF), lithium, all-trans-retinoic acid, minocycline, and oral
contraceptives.
Pathogenesis: The pathomechanism of Sweet’s syndrome is
theorized to involve the secretion of a neutrophilic chemoattractant factor,
which causes massive amounts of neutrophils to migrate into the skin. The exact
molecule responsible for the recruitment of neutrophils into the skin is
unknown. Reports of exogenous use of G-CSF have led to the theory that it is
responsible for the chemoattraction of neutrophils. Other chemoattractants are
possible players in the pathogenesis, including interleukin-8.
Histology: Histological examination shows massive dermal
edema with a dense infiltrate composed entirely of neutrophils. Varying amounts
of leukocytoclasis are present. Subepidermal bulla formation is possible
because of the extensive dermal edema. Special stains for microorganisms must
be negative to exclude an infectious process, and these must be backed up with
cultures to help disprove an infection, because the histological picture can
mimic an infectious process.
Treatment: Treatment
should be directed at the causative agent. Supportive care is needed for those
with postinfectious Sweet’s syndrome. Topical and oral steroids can
dramatically shorten the course of the disease. Sweet’s syndrome that develops
as a paraneoplastic process secondary to underlying leukemia should be treated
with oral or intravenous steroids once an infectious process has been ruled
out. This can result in a rapid response, but it is short lived once the
steroids are removed. True remission occurs only if the cancer is treated and
put into remission.