Metabolic
Bone Disease Primary Osteoporosis
Osteoporosis is a common
disease of the elderly, affecting over 2 million women in the UK, and
associated with significant morbidity and mortality. It is characterized by
‘fragility fractures’, defined as a fracture occurring after a fall from
standing height or less and it is estimated that 33% of women and 20% of men
over the age of 80 will sustain a hip fracture due to osteoporosis. Other
common sites for osteoporotic fractures include the spine and distal radius
(Colles’ fracture) and it is estimated that the cost to the UK National Health
Service and social services of treatment for osteoporotic fractures of the hip
alone is in the order of £2.3 billion per annum. Primary osteoporosis in women
is due to a combination of age and estrogen deficiency; the cause in men is
less clear but probably includes age-related falls in both estrogen and
androgen concentrations.
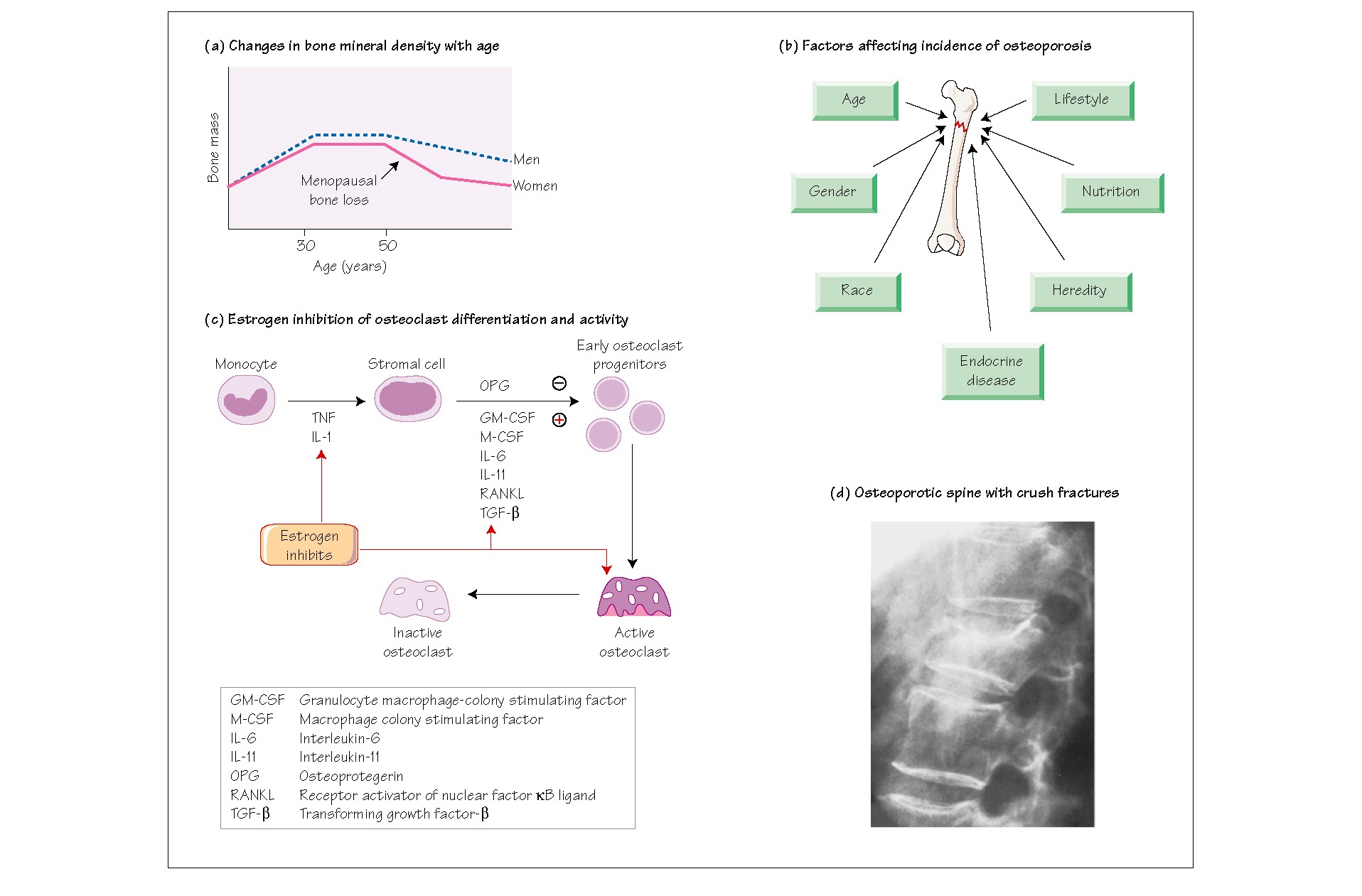
Osteoporosis occurs in the
context of lifetime changes in bone density. Peak bone density in both males
and females is achieved in the late 20’s and age-related bone loss begins at
the start of the fifth decade. Peak bone mass is genetically determined and a
major predictor of osteoporosis risk in later life. Other factors include sex
hormone status, nutrition, calcium and vitamin D status and levels of physical
activity. Both men and women exhibit age-related bone loss from the fifth
decade, but the process in women is accelerated during the menopause,
reflecting the role of estrogen as a major factor in the maintenance of bone
mineral density. Osteoporosis is diagnosed by assessing bone mineral density by
means of dual-energy X-ray absorptiometry (DEXA) scanning. The patient’s score
is measured according to standard deviation scores below normal peak bone mass.
A number of risk factors for
osteoporosis have been identified and include age, sex, family history,
Caucasian or Asian ethnicity, history of thyroid disease, cigarette smoking and
excessive alcohol intake. The major risk factor for fractures in the elderly
with osteoporosis is falling. Assessment of the patient should always include
risk factors for falling such as visual impairment, cardiovascular disease with
syncope, neuromuscular weakness and environmental hazards such as steps or
poorly fitting carpets.
Therapeutic intervention may
be offered as primary prevention to postmenopausal women, with significant risk
factors depending upon their bone density and as secondary prevention following
a fracture (see Chapter 55).
Aetiology
Osteoporosis is loss of bone
mass and is the most common metabolic bone disease. Gender, race, heredity,
lifestyle and nutrition, particularly the degree of calcium intake during the
period of peak bone growth, determine the incidence of osteoporosis (Fig. 54b).
The main phases of bone mass change are:
(i) attainment of peak bone
mass during postpubertal life and completion of bone mass consolidation between
the ages of 20 and 30; (ii) commencement of bone loss between the ages of 30
and 40, which occurs equally in trabecular and cortical bone approximately 25%
of bone is lost; and (iii) postmenopausal loss of bone, mainly trabecular (e.g.
vertebral), secondary to estrogen loss (Fig. 54a).
People of African Caribbean
origin have, on average, a higher peak bone mass than other ethnic groups.
Mother daughter and twin studies suggest that hip fracture is more likely when
there is a maternal history of osteoporosis, which may be accounted for by
inheritance of polymorphic alleles of the vitamin D receptor gene in some
populations. Nutritionally, an adequate intake of calcium by growing children
and young adults is critical in the attainment of genetically determined peak
bone mass, and calcium supplements have been shown to slow the rate of bone
loss in the elderly, although it is not certain whether calcium supplements
reduce the risk of fractures.
Exercise is an important
factor in determining the rate of loss of bone mass with ageing in both men and
women, and in both pre and postmenopausal women. The risk of hip fractures may
be reduced through regular exercise, although it is not clear whether this is
due to maintenance of adequate bone density or to maintenance of agility,
balance and muscle strength. Smoking has been shown to increase the rate of
metabolism of exogenous estrogens (for example in oral contraceptives),
although it is not known if smoking has this metabolic effect on endogenously
produced estrogens. A history of thyrotoxicosis is a risk factor for
osteoporosis.
Recent studies have found
evidence that 5-HT in the gut slows or may even stop phosphate uptake in the
gut. This is being actively studied and could conceivably generate novel
treatments to supplement mainstream treatments of osteoporosis.
Estrogen and osteoporosis
Osteoporosis through estrogen
deficiency is not age-dependent; accelerated bone loss may occur in hypogonadal
women of whatever cause. After menopause, there is an acceleration of bone
resorption due to estrogen deficiency, detected at biopsy as increased
activation frequency of basic multicellular units on bone and increased
resorption surfaces. There is increased excretion of metabolites of collagen
and bone and a moderate depression of PTH secretion. The coupling mechanism of
remodelling is maintained, with significant increases in levels of serum
alkaline phosphatase, osteocalcin and bone-specific alkaline phosphatase. All
these are indices of high bone turnover rates. Estrogen dampens osteoclast function
partly through inhibition of monocyte activation and of osteoblast activity
through suppression of genes that express IL-1, IL-6 and TNF (Fig. 54c).
The onset of osteoporosis is
often painless and insidious and, unless routine bone scans are done, the first
symptoms are due to the fracture. Spinal fractures in particular may be
painless, or present as persistent back pain that is relieved by bed rest and
exacerbated by any weight-bearing action (Fig. 54d). Fracture healing brings
remission from pain. With multiple compression fractures of the spine a sharply
localized forward angulation, called kyphosis, may result. The deformity is
caused by collapse of the anterior section of the vertebra. Appendicular
osteoporotic fractures (fractures of the limb bones) are often characterized by
fractures of the distal radius and the femoral neck.
Imaging studies and
laboratory findings
Bone densitometry is a
reliable diagnostic tool. It measures the total bone density or calcium content
at the wrist, spine and hip. The margin of error is small (1–2%) and the
radiation dose administered is a fraction of that given by X-ray. Other methods
include quantitative computed topography, which is more precise for cancellous
than for compact bone. X-rays are used but are less sensitive and can give
false positives since over-pentetrated films may misrepresent a normal spine as
osteopenic. Osteoporosis will not be detected by X-ray until approximately
35–55% of bone mass is lost.
Laboratory parameters
Osteocalcin and bone-specific
alkaline phosphatase, markers of bone formation, may be raised. Hormonal
indices in blood more often reflect age-related changes than any that might be
associated with osteoporosis. Serum levels of 1,2,5(OH)2D may be
lower in patients with osteoporosis but this is more likely to be due to the
reduction observed with ageing, and explained by reduced renal mass. Overall,
serum chemistry values are normal in patients with osteoporosis. Alkaline
phosphatase levels are raised when there is bone healing after osteoporotic
fractures.