Wrist And Forearm
Injuries
Injuries to the wrist and forearm are common,
often resulting from a fall onto an outstretched hand (FOOSH). It can be
difficult to distinguish subtle fractures from soft tissue injury on clinical
history and examination alone, so X-ray is usually necessary.
Fractures of
normal bones imply high-energy injuries, whereas a fracture occurring as
a result of a low-energy injury implies poor bone quality – a ‘fragility
fracture’, and the need to screen for osteoporosis.
In any
injury affecting the upper limb, dominance (handedness) and occupation and
hobbies must be recorded. If the injury is the result of a fall, consider
further investigations (Chapter 30).
Examination: look, feel, move
Compare with
opposite side, and look for swelling/bruising. A full range of elbow flexion,
pronation and supination makes significant injury unlikely. The radial, median
and ulnar nerve function in the hand should be checked (Chapter 14).
Management of fractures: principles
Pain should
be controlled by splintage and analgesic drugs before imaging. Elevation of the
arm in a sling reduces soft tissue swelling and pain. If there is any
evidence of neurovascular deficit or tenting of the skin by fractures, urgent
reduction will be necessary.
If there is
a skin wound over a fracture, this makes it an open fracture.
Antibiotics ± anti-tetanus treatment
must be given immediately. The wound should be covered with a
saline-soaked dressing, and the patient should go to theatre for debridement as
soon as possible.
Plaster of
Paris casts are used to hold the fracture in position while it heals. Rings
should be removed before plaster is applied, as the digits will swell.
Compartment
syndrome results from swelling of muscle within fascia compartments, e.g. of the
forearm, leg or foot. If untreated, the muscle dies, resulting in untreatable
ischaemic contracture. Patients should be warned about the symptoms: numbness,
pain and cold digits. If a patient has pain on passive stretching of a muscle,
compartment syndrome is likely; a palpable pulse does not exclude compartment
syndrome. If elevation does not solve the problem, the plaster must be
released, and a surgeon must review.
Common diagnoses
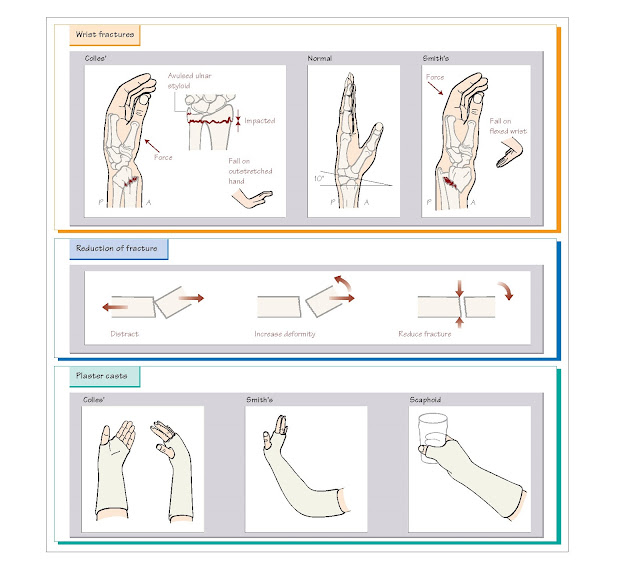
Colles’ fracture
This is a
fracture of the distal radius occurring in osteoporotic bone resulting
from low-energy impact, e.g. FOOSH. The fracture may be impacted and the
tip of the ulna is often avulsed. Dorsal angula- tion gives the wrist a ‘dinner
fork’ appearance.
The fracture
should be reduced in the Emergency Department using haematoma block and nitrous
oxide, or intravenous regional anaesthesia (Chapter 5). Good wrist function
depends on restoration of the length of the radius, and avoidance of steps in
the articular surface. On the lateral X-ray view, the articular surface of the
radius is normally 10° angulated towards the palm. This is often difficult to
achieve by reduction, but a neutral (0°) position is satisfactory.
High-energy distal radius fracture
This injury
occurs in normal bones as a result of high-energy impact, e.g.
falling off a bicycle. In comparison to a Colles’ fracture, there is more
likely to be comminution (multiple bone fragments), more soft tissue damage and
more pain: intravenous opiates are necessary.
To achieve
good function, these fractures need excellent (‘anatomical’) reduction and may
ultimately require operative fixation with plates or wires. A good reduction in
the Emergency
Department
using intravenous regional analgesia or procedural sedation (Chapter 6)
minimises soft tissue swelling and may avoid the need for further intervention.
Smith’s fracture
A Smith’s
fracture is sometimes called a reverse Colles’ fracture: it is a distal radius
fracture, but instead of dorsal angulation, there is volar (palmar) angulation.
However, Smith’s fractures often occur in normal bone, when they are high-energy
injuries. The structures on the volar (palmar) side of the wrist are at
risk of injury, particularly the median nerve.
A Smith’s
fracture is inherently unstable, and almost always needs open reduction and
internal fixation (ORIF) (e.g. with a plate and screws), although a good
reduction in the Emergency Department is usually the first step in the
management.
Diagnoses not to miss
Scaphoid fractures
The
difficulty in diagnosis and the consequences of failure to diagnose make this
fracture a frequent source of litigation. The history is usually FOOSH, and
clinical signs are pain:
• In the ‘anatomical snuffbox’ between extensor pollicis longus (EPL) and
abductor pollicis longus (APL).
• On axial thumb compression.
• On pressing over the scaphoid tubercle.
A patient with
clinical signs of scaphoid injury requires a ‘scaphoid view’ X-ray. If this
demonstrates a fracture, the joint should be immobilised as shown opposite.
Even if the
X-ray does not show a fracture, the patient should still be immobilised
in a splint or plaster cast, and sent home to have a definitive investigation,
e.g. repeat X-ray, in 1 week, or CT or MR scan, to prove or refute the
diagnosis of scaphoid fracture.
The reason
for this approach is that 20% of patients have fractures of the scaphoid that
are not visible on plain X-ray until at least 1 week after injury. If
the scaphoid fracture is missed, avascular necrosis and non-union can result in
early osteoarthritis and disabling stiffness of the wrist.
If you
perform an X-ray of the scaphoid, it is illogical and therefore medicolegally
indefensible not to follow up with a definitive investigation.
Fractures of shaft of radius and
ulna
The X-ray
must include the joint above and below to ensure that there is no dislocation.
These fractures need ORIF.
• Nightstick fracture: a mid-shaft transverse fracture of the ulna,
usually a ‘defence injury’ when the forearm is raised to protect the head
(‘nightstick’ is the US term for a police truncheon). Consider possible causes,
e.g. domestic violence.
• Monteggia fracture: fracture of proximal third of ulna and
dislocation of the head of the radius at the elbow.
• Galeazzi fracture: fracture of distal third of radius with associated dislocation
of distal radio-ulnar joint; rare.