SQUAMOUS CELL
CARCINOMA
Squamous cell carcinoma (SCC) of the skin is the second most common skin
cancer after basal cell carcinoma. Together, these two types of carcinoma are
known as non-melanoma skin cancer. SCC accounts for approximately 20% of all
skin cancers diagnosed in the United States. SCC can come in many variants,
including in situ and invasive types. Bowen’s disease, bowenoid papulosis, and
erythroplasia of Queyrat are all forms of SCC in situ. A unique subtype of SCC
is the keratoacanthoma. Invasive SCC is defined by invasion through the
basement membrane zone into the dermis. SCC has the ability to metastasize; the
most common area of metastasis is the local draining lymph nodes. Most forms of
cutaneous SCC occur in chronically sundamaged skin, and they are often preceded
by the extremely common premalignant actinic keratosis.
 |
Genital
Squamous Cell Carcinoma
Clinical Findings: SCC of the skin is most commonly located on the
head and neck region and on the dorsal hands and forearms. These are the areas
that obtain the most ultraviolet sun exposure over a lifetime. This type of
skin cancer is more common in the Caucasian population and in older
individuals. It is more prevalent in the fifth to eighth decades of life. The
incidence of SCC increases with each decade of life. This form of non-melanoma
skin cancer is definitely linked to the amount of sun exposure one has had over
one’s lifetime. Fair-skinned individuals are most commonly affected. There is a
slight male predilection. Other risk factors include arsenic exposure, human
papillomavirus (HPV) infection, psoralen + ultraviolet A light (PUVA) therapy,
chronic scarring, chronic immunosuppression, and radiation exposure. Transplant
recipients who are taking chronic immunosuppressive medications often develop
SCCs. Their skin cancers also tend to occur on the head and neck and on the
arms, but in addition they have a higher percentage of tumors developing on the
trunk and other non–sun-exposed regions.
SCCs of the skin can occur with
various morphologies. They can start as thin patches or plaques. There is
usually a thickened, adherent scale on the surface of the tumor. Variable
amounts of ulceration are seen. As the tumors enlarge, they can take on a
nodular configuration. The nodules are firm and can be deeply seated within the
dermis. Most SCCs are derived from a preexisting actinic keratosis. Patients
often have chronically sun-damaged skin with poikilodermatous changes and
multiple lentigines and actinic keratoses. Approximately 1% of actinic keratoses
per year develop into SCC.
Subungual SCC is a difficult diagnosis
to make without a biopsy. It is often preceded by an HPV infection, and the
area has often been treated for long periods as a wart. HPV is a predisposing
factor, and with time a small percentage of these warts transform into SCC.
This development is usually associated with a subtle change in morphology.
There tends to be more nail destruction and a slow enlargement over time in the
face of standard wart therapy. Prompt biopsy and diagnosis can be critical in
sparing the patient an amputation of the affected digit.
A few chronic dermatoses can
predispose to the development of SCC, including lichen sclerosis et
atrophicus, disseminated and superficial actinic porokeratosis, warts, discoid
lupus, long-standing ulcers, and scars. Many genetic diseases can predispose to
the development of SCC; two of the best recognized ones are epidermodysplasia
verruciformis and xeroderma pigmentosum.
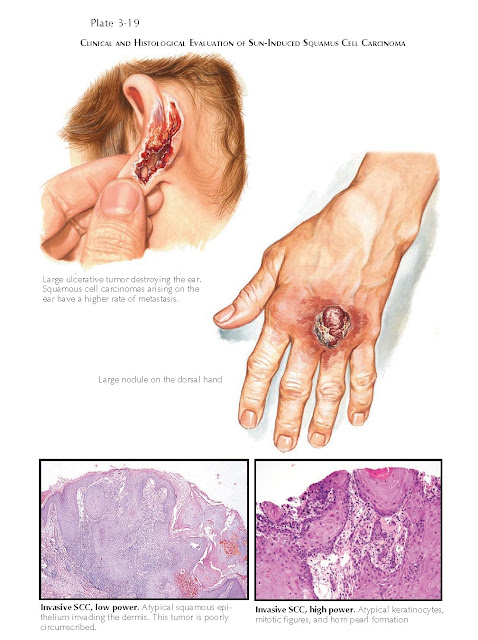 |
Clinical
And Histological Evaluation Of Sun-Induced Squamus Cell Carcinoma
Pathogenesis: SCC is related to cumulative ultraviolet exposure.
Ultraviolet B (UVB) light appears to be the most important action spectrum in
the development of SCC. UVB is much more potent than ultraviolet A light. UVB
can damage keratinocyte DNA by causing pyrimidine dimers and other DNA
mutations. The damaged DNA leads to errors in translation and transcription and
ultimately can lead to cancer. The p53 gene (TP53) is one of the
most frequently mutated genes. This gene encodes a protein that is important in
cell cycle arrest, which allows for DNA damage repair and apoptosis of those
cells that have been damaged. If the p53 gene is dysfunctional, this
critical cell cycle arrest period is bypassed, and the cell is allowed to
replicate without the normal DNA repair mechanisms acting on the damaged DNA.
This ultimately leads to unregulated cell division and cancer.
Histology: Actinic keratosis shows partial-thickness atypia
of the lower portions of the epidermis. The adnexal structures are spared. SCC
in situ shows full-thickness atypia of the epidermis that also affects the
adnexal epithelium.
SCC is derived from the keratinocytes.
The pathological findings are characterized by full-thickness atypia of the
epidermis and invasion of the abnormal squamous epithelium into the dermis.
Variable numbers of mitoses are seen, as well as invasion into the underlying
subcutaneous tissue. Horn pearls are often seen throughout the tumor. The
tumors are often described as being well, moderately, or poorly differentiated.
Many histological subtypes of SCC have been reported, including clear cell,
spindle cell, verrucous, basosquamous, and adenosquamous cell carcinomas.
Treatment: Actinic keratoses can be treated in myriad ways.
Cryotherapy with liquid nitrogen is very effective and can be used repeatedly.
If this fails to clear the area, or if the actinic keratoses are numerous,
medical therapy is often given with 5-fluorouracil (5-FU) or imiquimod. These
creams work, respectively, by directly killing the affected cells or by causing
the immune system to attack and kill the affected cells. They are both highly
effective. The disadvantage is that they cause an inflamma- tory response that
can be severe and cause erythema, crusting, and weeping during the period of
application, usually 1 month or longer.
The treatment for SCC in situ is often
electrodessication and curettage or simple elliptical excision. 5-FU cream is
also effective but leads to a higher rate of recurrence than the traditional
surgical methods. 5-FU is appropriate as a first-line agent for bowenoid
papulosis. If in follow-up any residual areas are left, surgical removal is
indicated. Occasionally, large areas of SCC in situ on the face are treated by
the Mohs surgical technique.
Invasive SCC should be treated surgically,
with Mohs surgery for lesions on the face or recurrent lesions; standard
elliptical excision is adequate for most invasive SCCs. Some small,
well-differentiated SCCs have been treated successfully with electrodessication
and curettage. The metastatic rate for cutaneous SCC is low, but certain
locations have a higher rate of metastasis. These areas include the lip, the
ear, and areas of chronic scarring or ulceration in which the tumors develop.
Recurrent SCCs, those larger than 2 cm in diameter, and those developing in
patients taking chronic immunosuppressive medications pose a higher risk for
the development of metastatic disease. Patients with chronic lymphocytic
leukemia (CLL) are at much higher risk for metastases; the reason is unknown
but is thought to be related to the immunosuppression resulting from their CLL.
The most common areas for metastasis are the local lymph nodes and lung.
Metastatic SCC of the skin should be
treated with adjunctive radiotherapy and chemotherapy. However, these therapies
have not shown a clear survival benefit, and the key to treatment ultimately
lies in the prevention of metastasis.




