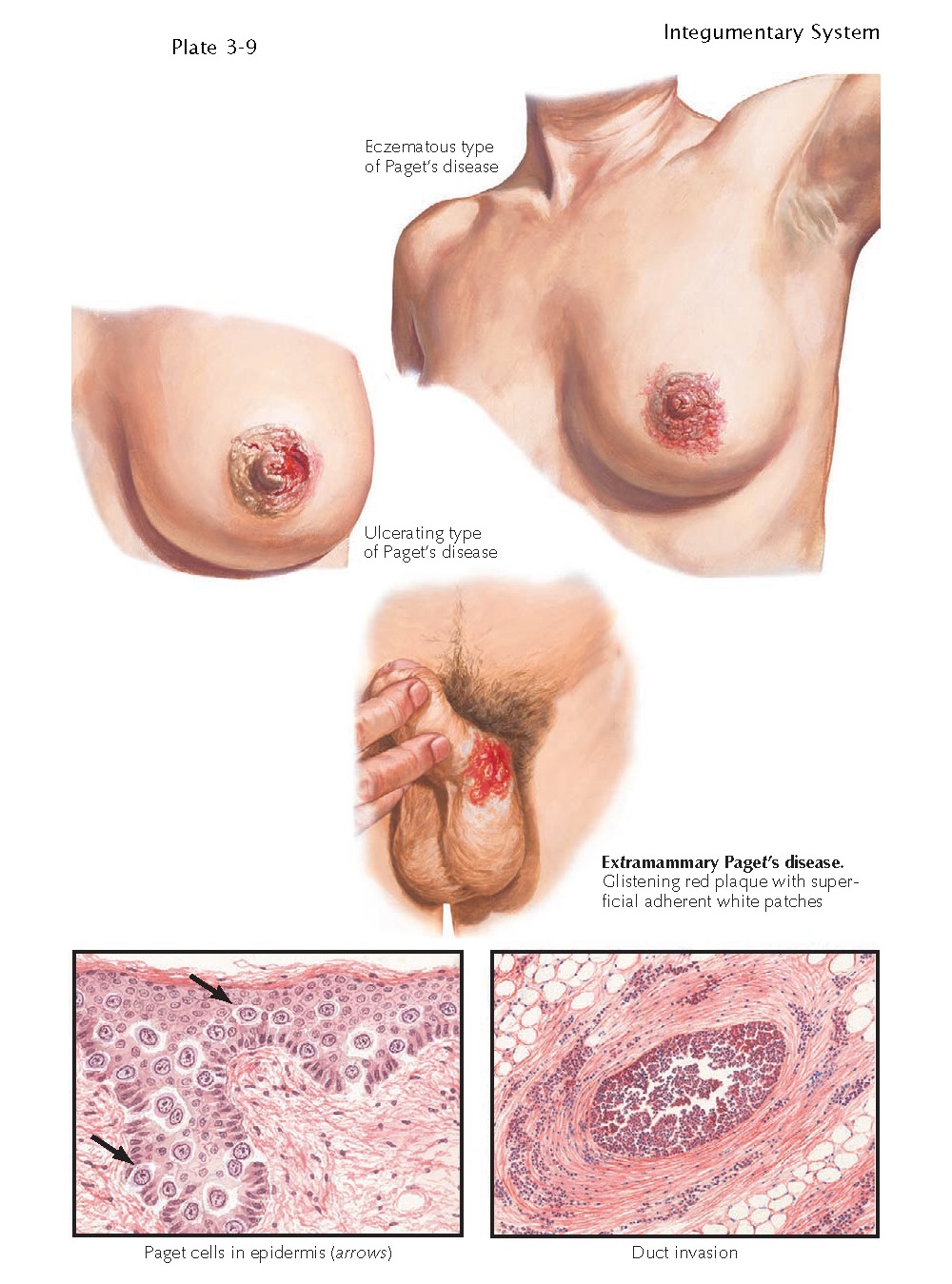
MAMMARY AND
EXTRAMAMMARY PAGET’S DISEASE
Extramammary Paget’s disease is a rare malignant
tumor that typically occurs in areas with a high density of apocrine glands. It
is most commonly an isolated finding but can also be a marker for an underlying
visceral malignancy of the gastrointestinal or genitourinary tract. Paget’s
disease is an intraepidermal adenocarcinoma confined to the breast; it is
commonly associated with an underlying breast malignancy.
Clinical Findings: Extramammary Paget’s disease is most often found
in the groin or axilla. These two areas have the highest density of apocrine
glands. It is believed that extramammary Paget’s disease has an apocrine
origin. There is no race predilection. These tumors most commonly occur in the
fifth to seventh decades of life. Women are more often affected than men. The
diagnosis of this tumor is often delayed because of its eczematous appearance.
It is often misdiagnosed as a fungal infection or a form of dermatitis. Only
after the area has not responded to therapy is the diagnosis considered and
confirmed by skin biopsy.
The tumor is slow growing and is
typically a red-pink patch with a glistening surface. Itching is the most
common complaint, but patients also complain of pain, burning, stinging, and
bleeding. The area is sore to the touch, and there are areas of pinpoint
bleeding with friction. The red, glistening surface often has small white
patches. This has been described as the “strawberries and cream” appearance,
and it is characteristic of extramammary Paget’s disease. As the cancer
progresses, erosions develop within the tumor, and occasionally ulcerations
form. The clinical differential diagnosis is often among Paget’s disease, an
eczematous dermatitis, inverse psoriasis, and a dermatophyte infection. A skin
biopsy is required for any rash in these regions that does not respond to
therapy.
The tumor is often a solitary finding;
however, it can be seen in conjunction with an underlying carcinoma, most commonly
adenocarcinoma of the gastrointestinal or genitourinary tract. Rectal
adenocarcinoma has been the most frequently reported underlying tumor. The
percentage of these tumors that are associated with an underlying malignancy is
not known but is estimated to be low. Appropriate screening tests must be
performed to evaluate for these associations. Usually, the underly- ing tumor
is diagnosed before the extramammary Paget’s disease or at the same time of
diagnosis.
Pathogenesis: The exact mechanism of malignant transformation is
unknown. Two leading theories exist as to the origin of the tumor. The first is
that the tumor represents an intraepidermal adenocarcinoma of apocrine gland
origin. The second theory is that an underlying adenocarcinoma spreads to the
skin and forms an epidermal component that manifests as extramammary Paget’s
disease. Although most believe this tumor to be of apocrine origin, controversy
surrounds this theory, and the exact cell of origin is still unknown. There are
no known predisposing factors.
Histology: The histology is diagnostic of the disease;
however, the pathological appearance often mimics that of melanoma in situ or
squamous cell carcinoma. There are a plethora of pale-staining Paget’s cells
scattered throughout the entire epidermis. This type of pagetoid spread of
cells is often seen in melanoma. The cells can be clustered together and can
have the appearance of forming glandular structures. Immunohistochemical
staining is often used to differentiate melanoma and squamous cell carcinoma
from extramammary Paget’s disease. Extramammary Paget’s disease is unique in
that it stains positively with carcinoembryonic antigen (CEA) and also with
some low-molecular-weight cytokeratins. It does not stain with S100, HMB-45, or
melanin A. The staining pattern with cytokeratins 7 and 20 has been used with
some success to predict an underlying adenocarcinoma; however, the routine use
of these tests is not clinically useful at this time.
Treatment: The prognosis for extramammary Paget’s disease
depends on the stage of the tumor. Disease that is localized to the skin has an
excellent prognosis. The treatment of choice is wide local excision. The risk
of recurrence is high, and lifelong clinical follow-up is required. The
prognosis for disease associated with an underlying adenocarcinoma is dependent
on the stage of the underlying tumor. Lesions associated with an underlying
malignancy have a worse prognosis. Metastatic disease has a poor prognosis, and
various chemotherapeutic reg mens have been tried with and without
radiotherapy.