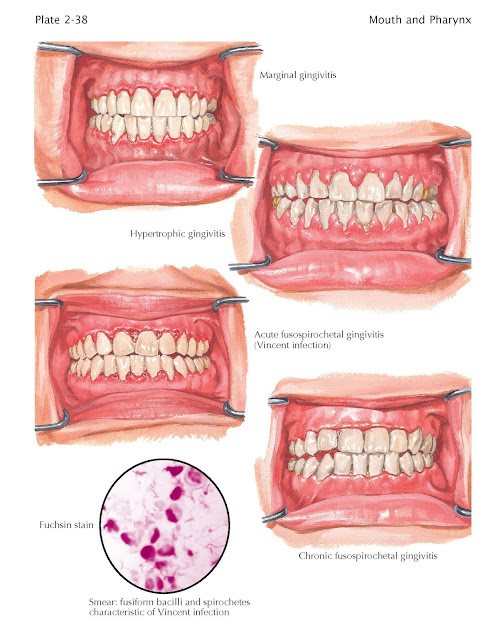
Gingivitis
Marginal
gingivitis is chiefly caused by
local irritating factors, such as calcareous deposits on the teeth, food
impaction, rough or overhanging filling margins and other dental restorations,
misalignment of teeth, open contacts or other morphologic faults causing
improper function, and hygienic neglect. These factors are, of course,
complicated by such conditions as allergies, mouth breathing, medications,
tobacco smoking, and hormonal changes. As with periodontal disease, individuals
may be genetically predisposed to the development of this condition. Marginal
gingivitis is the first stage in a complex periodontal syndrome that is further
characterized by pocket formation and inflammation of the investing tissues
(periodontitis) and, finally, by periodontal abscesses (see Plate 2-36).
Clinically, the gingiva is conspicuous for a shiny pink, red, or even cyanotic
surface, edema, and a strong bleeding tendency of the margins and papillae of
the gum. In the initial stages of the condition, there is a deepening of the
sulcus between the tooth and the gingiva; this is followed by a band of
erythema, indicative of the inflamed gingiva, which can be along one or, most
often, multiple teeth, resulting in edema of the inter- dental papillae that
easily induces bleeding.
Hypertrophic gingivitis describes a frequent variation of the marginal
type of inflammation, depending upon the individual response and the
chronicity. An increase in size of the papillae is more noticeable than that of
the free margin of gum and is especially related to accretions of calculus on
the teeth. Hormonal alterations, as in menstruation, pregnancy, and menopause,
will increase the degree of hypertrophy. Diffuse, idiopathic fibromatosis of
the gingiva, which is free of inflammation, is normal in color, and presents a
uniform proliferation of the gingiva in a firm, bulging mass throughout the
jaw, is another form of hypertrophic gingivitis; it is similar to the gingival
hyperplasia resulting from use of phenytoin.
Although the most common form of
gingivitis, plaque-induced gingivitis, is limited to gingivitis associated with dental plaque and is distinct from other presentations of gingivitis,
the bacterial plaque initiates the host response. The plaque accumulates in the
interdentition gaps, the gingival grooves, and plaque traps that harbor plaque.
The bacteria in the plaque activate lipopolysaccharides or lipoteichoic acid,
which promotes the inflammatory response causing gingival hyperplasia. As the
disease progresses, the bacterial situation becomes more complex, with an
increase in numbers and types of bacteria present.
Necrotizing ulcerative gingivitis, or fusospirochetal gingivitis, commonly known as
trench mouth, is a noncontagious opportunistic infection caused by bacte- ria
indigenous to the mouth in a host with reduced tissue resistance. Predisposing
factors include tobacco smoking, viral respiratory illnesses, poor nutritional
status, psychological stress, and immunocompromised states such as HIV/AIDS.
Chemoradiation therapy may also be a predisposing factor. Local causes include
all conditions promoting growth of anaerobic organisms, such as gum flaps over
third molar teeth, crowded and malpositioned teeth, inadequate contact areas,
food impaction areas, and poor oral hygiene.
The flora of necrotizing ulcerating
stomatitis typically includes one or more types of spirochetes and a fusiform
bacillus. Ulceration and pseudomembrane formation are the specific lesions seen
in this condition.
The acute form presents with a sudden
onset of oral pain and constitutional symptoms of elevated temperature and
malaise; it is more often seen in children or immunocompromised individuals.
Submandibular lymphadenopathy is variable. Severe pain, a strong characteristic,
malodourous breath, and gingival bleeding are marked; objectively, these signs
are related to flat, punched-out, grayish ulcers, which erode the tips of the
papillary gingivae and spread to the margins, which are covered by a thin
diphtheritic-like membrane. On slight pressure, bleeding may occur from all
affected areas. In severe cases the lesions spread to the tongue, palate,
pharynx, and tonsils; profuse salivation, a thickly coated tongue, and bleeding
are seen.
Chronic necrotizing gingivitis is a milder form of this disease; it exists from
the outset or is a slowed down phase of the acute form. Subjective symptoms are
much reduced. The first awareness is of bleeding when brushing the teeth.
Careful retraction of the papillae may be necessary to reveal the typical
necrosis. Pain is usually absent. The typical odor develops later because
destruction proceeds slowly. The response to therapy is far slower in
long-established cases, and recurrence is a constant hazard. As the
architecture of the gingiva is altered, anaerobic areas are created and food
retention is abetted, so that therapy against the infection alone is of only
momentary value; it must be directed to a restoration of the proper gingival
form.