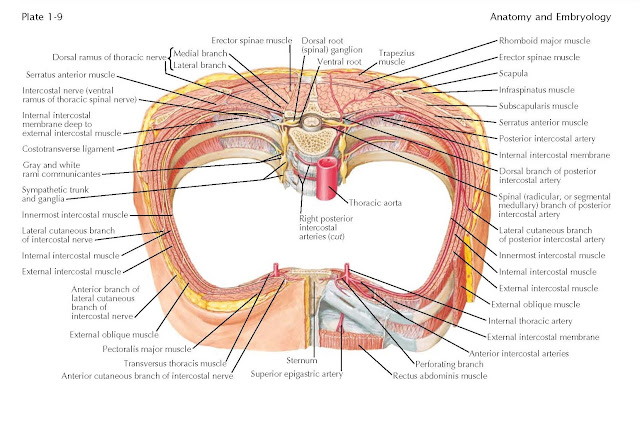
Intercostal Nerves And Arteries
The
typical thoracic spinal nerve is formed by the junction of a dorsal root and a
ventral root near the intervertebral foramen below the vertebra having the same
number as the nerve. The dorsal root is made up of a series of rootlets
that emerge from one segment of the spinal cord between its dorsal and lateral
white columns; it contains the nerve cell bodies of the afferent neurons that
enter the spinal cord through it. This collection of nerve cell bodies causes a
swelling of the root, named the dorsal root ganglion. A series of
rootlets composed of axons of ventral-born gray cells leaves the same segment
of the cord between the lateral and ventral white columns to form the ventral
root of the spinal nerve.
The dorsal and ventral roots join near the intervertebral
foramen to make up the very short common trunk of the spinal nerve,
which divides almost immediately into the dorsal ramus (posterior primary
division) and the ventral ramus (anterior primary division). The white and gray
rami communicantes, which connect the ganglia of the sympathetic trunk and the
thoracic nerves of the same level, join the ventral ramus near its origin.
The dorsal ramus of the thoracic nerve, passing
posteriorly, pierces the erector spinae muscle (which it supplies), the
trapezius muscle, and the other superficial muscles of the back (depending on
the level) to reach the superficial fascia. There it divides into a smaller
medial branch and a longer lateral cutaneous branch, which supply the skin.
The ventral ramus of the thoracic nerve is the intercostal
nerve of that particular level (for the twelfth thoracic nerve, the subcostal
nerve). From the seventh to the eleventh thoracic levels, the ventral rami of
the thoracic nerves continue from the intercostal spaces into the anterior
abdominal wall. The intercostal nerve runs forward in the thoracic wall between
the innermost intercostal muscle and the internal intercostal muscle. It lies
inferior to the intercostal vein and intercostal artery and gives off a
collateral branch to the lower part of the space, as do the vein and artery.
The intercostal nerve has a lateral cutaneous branch at the lateral aspect of
the thorax that pierces the overlying intercostal muscles to reach the
subcutaneous tissue. There it divides into an anterior (mammary) and a posterior
branch. At the anterior end of the intercostal space, the intercostal nerve
ends by becoming the anterior cutaneous nerve, which divides into a lateral
branch and a shorter and smaller medial branch.
The aorta, lying on the anterior aspect of the vertebral
bodies, gives off pairs of posterior (aortic) intercostal arteries. The right
posterior intercostal arteries lie on the anterior aspect and the right side of
the vertebral bodies as they travel to reach the intercostal spaces of the
right side. The right and left posterior intercostal arteries course forward in
the upper part of the intercostal spaces between the intercostal vein above and
the intercostal nerve below to anastomose with the anterior intercostal
branches of the internal thoracic and musculophrenic arteries. Collateral
branches run in the inferior parts of the intercostal space.
To reach the pleural cavity from the outside at the
anterolateral aspect of the thorax, a needle would pass through the following
layers: skin, superficial fascia, intercostal muscles and related deep fascial
layers, sub-pleural fascia, and parietal layer of the pleura. If the needle is
carefully inserted near the lower part of the intercostal space (i.e., above the
rib margin), one is reasonaly sure of avoiding the intercostal nerve and vessels.