Neurologic Conditions
Of The Shoulder
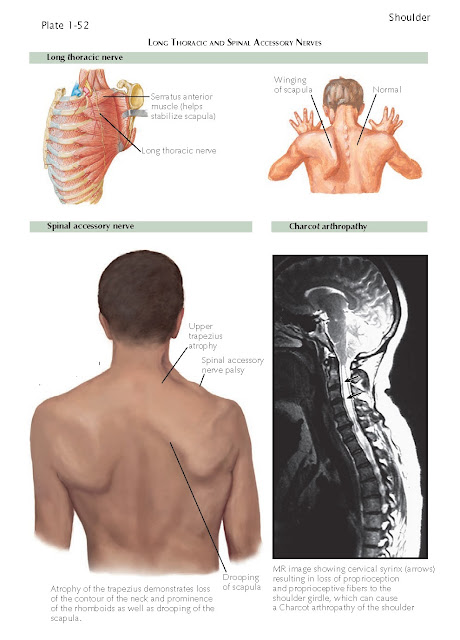
The long thoracic nerve innervates the serratus
anterior muscle (see Plate 1-13). The serratus anterior muscle has its origin
in the anterior chest wall and then inserts along the medial border of the
scapula with most of its fibers attaching to the distal third of the scapular
body (see Plate 1-13).
When there is a lesion of the long
thoracic nerve and weakness of the serratus anterior muscle, there is winging
of the scapula. When severe, there is limitation of active elevation of the
shoulder because of an unsta- ble scapula that is not able to appropriately
rotate laterally and maintain its position along the chest wall. In this particular
case, by using overactive rhomboid function and trapezius function the patient
is trying to compensate for loss of the function of the serratus anterior
muscle. When this lesion occurs as a result of a viral insult or closed trauma,
then spontaneous recovery often occurs over a period of several months to a
year. When recovery is either incomplete or results in significant long-term
disability, then pectoralis major muscle transfer to the tip of the scapula is
a well-defined and effective treatment.
Charcot arthropathy of the shoulder
can be associated with severe destructive lesions of both the humeral head
and glenoid and is often evident on radiographs as multiple-joint bony debris.
In some cases this is associated with a cervical syrinx, resulting in loss of
proprioception and proprioceptive fibers to the shoulder girdle. When there is
loss of sense of joint position, normal activities and pain associated with
injury are not perceived by the patient, resulting in severe destructive damage
to the joint. Often the patients have much less pain and better function then
what would be expected by the severity of the joint damage. Because of the
underlying cause of the shoulder damage, joint replacement or any type of
surgical reconstruction has a high rate of complications, including prosthetic
dislocation, periprosthetic fractures, and loosening of the prosthetic
components.
Suprascapular nerve lesions can be
associated with entrapment of the suprascapular notch or spinal glenoid notch.
They can also be associated with ganglion cyst formation. This will result in
weakness of external rota- tion and an external rotation lag sign (see Plate
1-40). Atrophy of the musculature of the supraspinatus fossa and infraspinatus
fossa should be evaluated. Ganglion cyst formation can be associated with a
superior labral tear (see Plate 1-51). The ganglion cyst forms as a synovial
fluid-filled sac. When this ganglion encroaches on the suprascapular notch or
spinoglenoid notch (see Plate 1-51) there is a suprascapular nerve compressive
neuropathy.
These lesions can be treated by
aspiration under image guidance. When treated by needle aspiration the ganglion
can recur because the SLAP lesion is not repaired. Arthroscopic repair of the
SLAP lesion can result in spontaneous resolution of the ganglion cyst.
Alternatively, the SLAP lesion can be repaired arthroscopically with excision
of the ganglion cyst. The clinical appearance for suprascapular neuropathy is
severe atrophy of the supraspinatus or infraspinatus musculature. Isolated
atrophy of the infraspinatus muscle is associated with entrapment of the
infraspina- tus branch of the suprascapular nerve at the spinoglenoid notch.
Lesions of the spinal accessory nerve
involve weakness or paralysis isolated to the trapezius muscle. Spinal accessory
nerve lesions can also be associated with viral syndromes. They can also be
seen as an iatrogenic lesion associated with cervical node biopsy. The shoulder
demonstrates drooping of the scapula, noted as one shoulder not being level to
the other, the neck contour is distorted, and the rhomboid muscles are
prominently seen because the middle trapezius is atrophied. This lesion also
causes winging of the scapula with predominate involvement of the upper half of
the scapula and can be distinguished from the long thoracic nerve palsy with
serratus anterior muscle weakness that affects predominately the lower pole of
the scapula. Chronic lesions that are associated with incomplete or lack of
recovery can be treated with transfer of the levator scapulae and rhomboid
musculature (Eden-Lang procedure). This is an effective muscle transfer as a
salvage procedure for this nerve and muscle lesion.