The Immunocompromised
Host
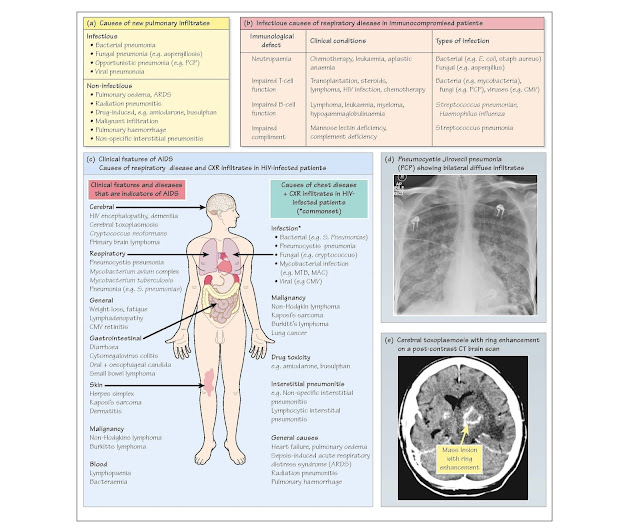
The immune system is most frequently impaired after chemotherapy and in
patients with human immunodeficien y virus (HIV) infection. Immunodeficien y
also occurs in patients with malignancies of the lym- phoproliferative system
(e.g. leukaemia), immediately following bone marrow transplants (BMT) and in
those on immunosuppressive drugs (e.g. steroids and azothioprine) particularly
after transplant surgery (e.g. renal). Malnutrition or chronic illness (e.g.
diabetes) may also impair immunity. Respiratory disease is particularly common
in the immunocompromised host.
Clinical presentation is often non-specifi (i.e. fever, dyspnoea, hy-
poxia, cough and chest discomfort) and investigation inconclusive making
diagnosis diff cult. In particular, pulmonary infiltrate are not always due to
infection (Fig. 39a). Clinical clues include rate of onset (i.e. rapid in
bacterial infection and slow with malignancy), drug therapy (e.g. methotrexate)
and extrapulmonary features (e.g. Kaposi's sarcoma). Establishing the diagnosis
may require invasive techniques (e.g. biopsy) with associated risks (e.g.
haemorrhage).
Investigations include blood and pleural fluid microscopy,
culture and serology. Sputum for Aspergillus or mycobacteria and
'induced' sputum for Pneumocystis jiroveci pneumoniae (PCP). CXR f
ndings may be non-specifi (e.g. diffuse infiltrates) Chest CT scans assess ex-
tent of lung involvement, aid invasive sampling and may be diagnostic (e.g.
halo sign of aspergillosis). Consider early bronchoalveolar lavage (BAL) with
microbiology, stains (e.g. fungus and virus), immunofluo rescence (e.g. PCP)
and serology (e.g. CMV and Cryptococcus) as this is often diagnostic
(50-60%). Transbronchial, f ne-needle and surgical lung biopsies have risks but
may aid diagnosis.
Diagnosis is due to respiratory infection in more than 75%
of cases:
· Infection depends on the immunological defect (Fig. 39b) and
prophylactic therapy (e.g. septrin for PCP).
· Non-infectious
causes present with similar
clinical and CXR features to infection and include pulmonary oedema, ARDS, malignancy
(e.g. lymphoma), diffuse alveolar haemorrhage, pulmonary embolism, drug-induced
disease (e.g. methotrexate), BMT-associated idiopathic pneumonia, radiation
pneumonitis and chronic graft-versus-host disease. More than one cause is often
present (30%).
Treatment is often empirical as antibiotic therapy cannot be
delayed in febrile neutropaenic patients, in whom infection is a medical
emergency. Blood cultures should always precede antibiotics.
· Antibiotic
choice depends on the clinical situation
and local antibiotic policy. Initial treatment of immunosuppressed cases
involves broad-spectrum antibiotics ( antiviral and antifungal agents).
Treatment should be adjusted when results are available. PCP and CMV therapy
have significan toxic side effects, but if suspicion is high, treatment is
started empirically. PCP can be diagnosed for up to 2 weeks after onset of
therapy. Treatment of mycobacteria is only started after definit ve diagnosis.
· Steroid
therapy is recommended in PCP,
radiation/drug-induced pneumonitis, BMT idiopathic pneumonia and alveolar
haemorrhage.
· Supportive
therapy includes supplemental
oxygen and ventilatory support. Respiratory failure has a poor outcome in these
patients.
Respiratory manifestations in the HIV-positive patient
(Fig. 39c)
Acquired immune deficien y syndrome
(AIDS) is due to infection with HIV, which impairs and depletes CD4
T-lymphocytes (Chapter 18). Reduction in T-lymphocyte availability predisposes
to viral or fungal infections and neoplasia (Fig. 39e). Highly active
antiretroviral therapy (HAART) allows T-lymphocyte population recovery, reduces
suscepti- bility to infection and improves survival. Nevertheless, HIV patients
are at increased risk of infection with common bacteria, PCP, mycobacteria and
fungi. Factors determining the type and risk of infection include the use of
prophylactic antibiotics (e.g. PCP prophylaxis), source of infection (e.g. TB
is more common with drug abuse) and geography (e.g. histoplasmosis and
coccidioidomycosis are more common in the USA). Extrapulmonary features (e.g.
Kaposi's sarcoma) may suggest the cause of pulmonary disease.
1. Infectious causes
· Bacterial pneumonia (e.g. Streptococcus pneumoniae, Staphylococcus
aureus and Nocardia) is the commonest chest infection in HIV
patients. Rapid onset of high fever, purulent sputum and pleuritic chest pain
help distinguish bacterial pneumonia from PCP. Legionella infections are
more common in HIV patients.
· Pneumocystis jirovecii pneumonia occurs in severely immunocompromised patients (CD4 <200 106/L).
It has been less common since the use of septrin prophylaxis in high-risk
cases. It presents with gradual onset of fever, dry cough, exertional dyspnoea,
chest tightness, tachypnoea and rarely pneumothorax. Exercise-induced
desaturation progresses to resting hypoxaemia. CXR shows bilateral alveolar
infiltrate (Fig. 39d) but may be normal (10%) or show focal consolidation.
Diagnosis requires detection of pneumocysts in induced sputum ( ̴60-70%) or BAL (>90%). High-dose
co-trimoxazole is the most effective therapy but may cause rashes ( ̴30%), vomiting and blood disorders. Pentamidine
and dapsone are second-line alternatives. High-dose steroids reduce alveolitis,
respiratory failure and mortality.
· Mycobacteria (e.g. Mycobacterium tuberculosis
(MTB), My- cobacterium avium complex (MAC)). Globally 10% of
MTB cases are also infected with HIV. However, co-infection rates vary
geographically affecting 35-40% in sub-Saharan cases and 2.7% in the UK. HIV
patients with previous MTB exposure have a 10% chance of reactivation, and
approximately 33% of patients exposed to MTB develop primary disease. Advanced
immunosuppression is typically associated with diffuse pulmonary involvement,
mediastinal adenopathy and extrapulmonary involvement. Symptoms may deteriorate
with the onset of HAART due to immune reconstitution. Non-tuberculous
mycobacterial (NTM) infection is due to MAC in more than 90% of cases. MAC
treatment is lifelong unless immune restoration is achieved with HARRT.
· Viral (e.g. influenz and herpes simplex). Cytomegalovirus (CMV) is
ubiquitous and normally harmless but can cause life-threatening pneumonia in
the immunocompromised. Diagnosis requires evidence of viraemia (i.e.
antigen/PCR testing on blood/BAL) or tissue invasion (e.g. 'owl eye' inclusion
bodies in infected biopsy cells). Ganciclovir is the most effective antiviral
agent.
· Fungal (e.g. Aspergillus). Cryptococcus neoformans propagates
asymptomatically in alveoli following inhalation (from bird drop-pings), before
migrating to the CNS where it causes meningitis ( ± encephalitis). Onset is acute
or chronic with fever, cough and non-specifi CXR changes. The cryptococcal
antigen test and India ink stain establish the diagnosis. Treatment is with
amphotericin, fluytosine and fuconazole. In endemic areas, histoplasmosis and
coccidioidomycosis may cause respiratory disease.
2. Non-infectious causes
· Malignancies are occasionally confused with infection in HIV patients. Kaposi’s
sarcoma is a tumour of vascular origin associated with human herpesvirus 8
infection. Clinical manifestations range from asymptomatic incidental discovery
to fulminating disease, causing respiratory failure. Non-Hodgkin’s lymphoma occurs
in advanced immunosuppression and is typically aggressive B-cell or Burkitt's
lymphoma, suggesting pre-existing herpesvirus infection. Lung cancer is
also increased in HIV patients.
· Interstitial pneumonitis (e.g. NSIP, LIP, Chapter 30).
· Drug-induced lung disease or heart failur