Oogenesis
Time period:
week 12 to menopause
Female germ
cells proliferate by mitosis in the ovaries to form a large number of oogonia.
These cells are diploid, contain two X sex chromosomes, and will become haploid
mature oocytes via the process of oogenesis. This process is similar to
spermatogene- sis but has some significant differences.
The germ
cells that will form the female gametes (oocytes) are derived from germ cells
that migrate from the yolk sac into the site of early gonad formation (see
Chapter 38).
The ovaries
are a pair of organs that produce oocytes and reproduc- tive hormones. They lie
near the openings of the uterine tubes (also known as the Fallopian
tubes or oviducts) that extend from the uterus. Finger‐like projections from
the uterine tubes called fimbriae collect oocytes when they are expelled from
the ovaries. The oocyte is carried into and along the uterine tube for
fertilisation and subse- quent implantation into the wall of the uterus.
The adult
ovary is predominantly made up of connective tissue that supports a large
number of follicles. Blood vessels and nerves are concentrated within the
central medulla whereas follicles are found in the outer cortex, in varying
stages of development.
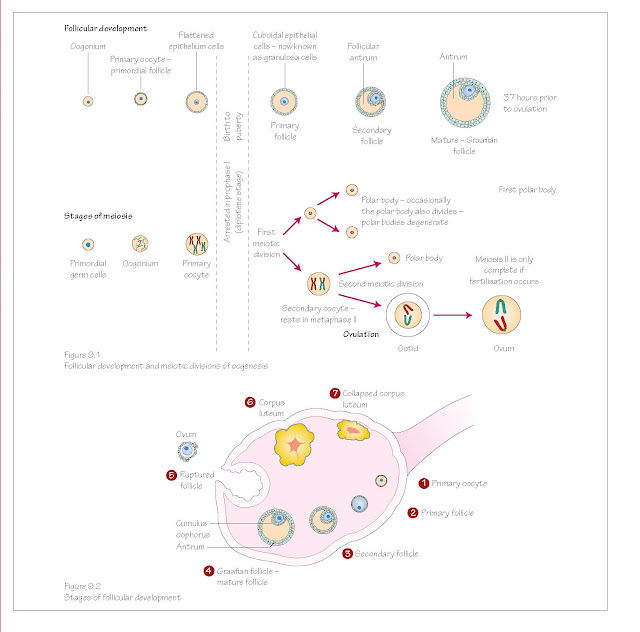
Meiosis I
Oogonia
begin oogenesis by entering meiosis I in week 12 of embryonic development
(Figure 9.1). During meiosis I the cell is known as the primary oocyte,
and is surrounded by a thin layer of squamous epithelial cells. This structure
is a follicle, and in its very early stage is called a primordial
follicle. The primary oocyte at this stage is developmentally arrested in
prophase of meiosis I. This pause in development may continue for 45 years or
more.
The number
of primordial follicles vastly increases during the foetal period but many
degenerate, leaving around 400,000 follicles available at puberty. After birth
no new oocytes form.
With the
onset of puberty some of the stalled primary oocytes continue oogenesis each
month (Figure 9.1).
The primary
oocyte becomes larger and the follicular cells around it become cuboidal and
the layer thickens. The follicle is now a primary follicle (Figure 9.2).
The oocyte
and the granulosa (follicle) cells produce a layer of glycoproteins on the
surface of the oocyte called the zona pellucida.
When the
follicle forms more than one layer of granulosa cells it is called a secondary
follicle.
One follicle
continues to develop and grow, and the others degen- erate. It is not clear how
one follicle is chosen over the others.
A cavity
called the antrum forms between the layers of granu- losa cells, and the
mass of follicular cells is now termed the cumulus oophorus.
The
connective tissue cells of the ovary around the follicle respond by
differentiating and forming two new layers: the theca interna and the theca
externa. The theca interna has a hormonal role, and the theca externa a
supportive role. This follicle is now a mature vesicular follicle or Graafian
follicle.
The thecal
and granulosa cells of the developing follicles pro- duce oestrogens that cause
the thickening of the endometrial lin- ing of the uterus and other preparations
for receiving a fertilised oocyte. This occurs from days 5 to 14 of the
menstrual cycle (see Figure 5.1 and Chapter 12).
The primary
oocyte of the Graafian follicle responds to surges in follicle stimulating
hormone (FSH) and luteinising hormone (LH) produced by the pituitary
gland on days 13–14 of the menstrual cycle by resuming meiosis I and continuing
its stalled cell division (Figure 9.1).
When the
oocyte divides it forms one large cell and one smaller remnant of the division
known as a polar body. At the end of meiosis I the oocyte has become a secondary
oocyte.
Polar bodies
are small, non‐functional cells. They receive very little of the available
cytoplasm and degenerate soon after division. In this way the oocyte is able to
retain its size but discard chromo- somal material to become a haploid cell
ready for fertilisation.
One polar
body is formed with meiosis I and two polar bodies are formed with meiosis II.
Meiosis II
The secondary
oocyte begins meiosis II but this division is again halted, this time during
metaphase II. Meiosis II will only continue if the oocyte is fertilised.
With
ovulation the secondary oocyte is passed into the uterine tube, but the
follicle remains within the ovary (Figure 9.2). At this stage the follicle is
very large and makes up a significant portion of the ovary. This follicle
becomes the corpus luteum.
In response
to LH the corpus luteum produces progesterone, oestrogens and other hormones
causing the endometrium of the uterus to thicken further, develop its
vasculature, form glands and prepare for implantation.
If
fertilisation does not occur the corpus luteum degenerates about 14 days later
and becomes a scar tissue remnant of itself called the corpus albicans.
Hormone production ceases and menstrua- tion begins as the thickened
endometrium is shed.
Clinical relevance
The primary
oocyte may be arrested in meiosis I throughout life for 40–50 years if it is
not triggered to continue development until a menstrual cycle late in
reproductive life. DNA fragmentation within those stored oocytes is more common
in older women as DNA damage increases with time. This may be the reason for
reduced fertility with increasing age.
Knowledge of
the sex hormones’ effects on follicle development have allowed the invention
of the oral contraceptive pill. High levels of oestrogens and progesterone
inhibit gonadotrophin releasing hormone (GnRH) and subsequently LH and FSH
release. Decreased levels of FSH mean that the follicle is not stimulated to
develop, and the absence of an LH surge prevents ovulation occurring.
Chemotherapy
and radiotherapy can destroy primordial ovarian follicles. As there is a finite
reserve of oocytes formed prenatally, which cannot be replenished after
treatment, the cryopreservation of oocytes before treatment begins should be
considered. Frozen ay be used for in vitro fertilisation at a later date
if the patient becomes infertile.