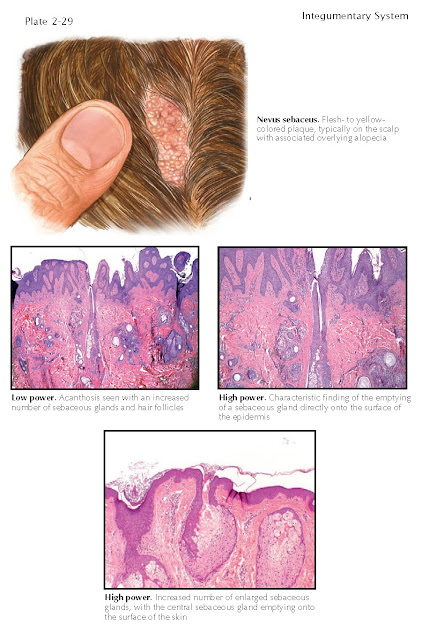
Nevus Sebaceus
Nevus sebaceus, also known as organoid nevus or
nevus sebaceus of Jadasshon, is a benign tumor that manifests in infancy or
early childhood. This tumor has a risk of malignant transformation after
puberty, and basal cell carcinoma is the malignant tumor that most frequently
develops within these lesions.
Clinical Findings: Most of these growths are very small, and some
escape detection for years. Others can be obvious at birth. They show a large
range in dimensions. Most are solitary. The most common location in which to
find a nevus sebaceus is within the scalp. Together, the scalp and face are
overwhelmingly the areas of involvement, and it is rare to find a lesion any
other place on the body. At or soon after birth, an area of the scalp is seen
to be obviously affected. Nevus sebaceus typically start off as a thin,
yellowish-brown patch or plaque. The area is almost universally devoid of
terminal hair shafts. With time, the area becomes more cobblestoned in
appearance. These nevi are usually asymptomatic but can be a cosmetic problem
depending on their size and exact location. They occur in males and females
with equal frequency. The lesions enlarge in proportion to the growing child.
Before puberty, the risk of malignant transformation is very low. After
puberty, approximately one third of these lesions develop a secondary growth,
which usually manifests as a new nodule within the nevus sebaceus. The nodule
can vary in color, but a light, translucent purple color is not infrequently
seen. It is also common for a bleeding nodule or papule to develop within the
underlying nevus sebaceus.
Most commonly, these growths that
occur within the nevus sebaceus are benign in nature. The syringocystadenoma
papilliferum is the most common benign tumor to develop within a nevus
sebaceus. Because of the connection to the epidermis, these growths usually
manifest as a draining or bleeding nodule that is slowly enlarging. The most
common malignant growth to develop in a nevus sebaceus is a basal cell
carcinoma. These usually manifest as a pearl-colored papule with a central
ulceration and varying amounts of bleeding or crusting. The transformation to
malignancy has been shown to increase with the age of the patient. It is
estimated that about 1% of nevus sebaceus lesions will develop a malignant
growth over the patient’s lifetime. There have been multiple reports of various
tumors arising within a nevus sebaceus, and there have also been reports of
multiple tumors arising within the same nevus sebaceus.
The nevus sebaceus syndrome is a very
rare finding. It is similar in nature to the epidermal nevus syndrome. This
syndrome can have a varying phenotype. The neurological system, including the
eye, and the musculoskeletal, cardiovascular, and genitourinary systems can all
be involved to varying degrees. Patients with this syndrome usually have
abnormally large areas of cutaneous involvement. The lesions can be found
anywhere on the body and are often multiple.
Pathogenesis: Nevus sebaceus is considered to be a hamartomatous
process of the epidermis and adnexal structures of the skin. The exact
mechanism and cause have not been discovered.
Histology: The histological picture is dependent on the age
of the patient. Before puberty, the findings are more subtle than after
puberty. Prepubertal lesions most commonly show undeveloped adnexal structures.
After puberty, the lack of terminal hair follicles is a universal finding. Fine
vellus hair follicles are often present but in reduced numbers. Prominent sebaceous
glands are seen. Many of the sebaceous glands empty directly onto the surface
of the epidermis. The overlying epidermis shows acanthosis and papillomatosis.
The presence of apocrine glands is often appreciated.
Treatment: If treatment is undertaken, complete surgical
excision is the treatment of choice. This not only removes the lesion but also
removes the risk of malignant potential. Another approach is to watch and wait,
with routine observation. If the nevus sebaceus develops any areas of change, a
prompt biopsy is warranted. The timing of the surgical removal is
controversial, and because the risk of malignancy is low, it is acceptable to
wait until the patient is old enough to make the decision. The size and
location of the nevus sebaceus dictates the type of surgical excision and
repair required. Treatment of the rare nevus sebaceu syndrome requires a
multidisciplinary team approach.