Diagnosis
The Emergency Department is a
diagnosis machine, taking people with a wide variety of symptoms, labelling
them with a diagnosis, treating and then discharging them whenever safe to do
so. There are plenty of opportunities for this process to go wrong, and it is
important to understand how this can occur.
Despite a couple of thousand years of medical education,
we are still not really sure how the diagnostic process works.
• Some people work forward from
history, examination and a shortlist of differential diagnoses.
• Others work backwards from a
list of likely diagnoses to weight these according to symptoms and examination.
•
Experts make their diagnoses by
pattern recognition.
It may be that expertise occurs with the development of
cognitive flexibility to use multiple diagnostic strategies to integrate and test the result.
Using tests
In the past, the Emergency Department used a few simple
tests to inform decision-making. An X-ray of an injured limb has a binary
outcome: broken/ not broken. As technology and the scope of Emergency Medicine
has increased, the tests have become more numerous and less black and white,
and there is a need to rationalise and manage the uncertainty generated.
The most common way of describing a test’s performance
is to use sensitivity and specificity.
For example, if a very specific test, e.g.
Troponin I, is positive, we know that myocardial damage has occurred, because
the number of false positives (B) is very low. Similarly, if a very sensitive
test, e.g. CT scan for abdominal aortic aneurysm (AAA), comes back as
negative, we know that it is very unlikely that the patient has an AAA as the
number of false negatives (C) will be very low.
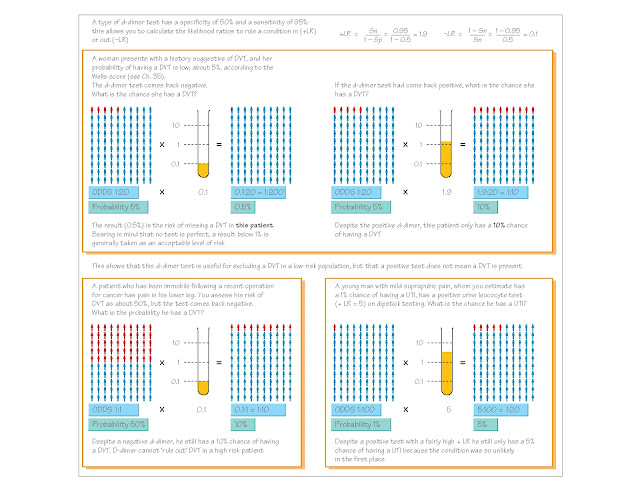
However, Emergency Departments use many tests that are
not 100% sensitive or specific, and therefore a more powerful, but less
intuitive, model is necessary to understand these tests: likelihood ratios,
which are calculated from the specificity and sensitivity.
Treatment orders
Once the likely diagnosis has been made, a set of
treatment orders needs to be decided and documented. A good acronym for this is
DAVID, e.g., for an elderly patient with an open fracture of the tibia:
•
Diet – nil by mouth
•
Activities – elevate limb
•
Vital signs monitoring – hourly limb observations
•
Investigations – CXR, FBC, U+E
•
Drugs/treatment – immediate i.v. antibiotics