Organ Allocation
There are many more people on the transplant waiting list than
there are organs available. To manage this shortage access to the waiting list
is restricted to those meeting strict eligibility rules. Once on the waiting
list allocation follows pre-defined rules to ensure fairness.
Eligibility for transplantation
Criteria vary from organ to organ, and country to country. In
addition, different considerations may be necessary for patients needing a
second transplant after the first has failed, particularly since for most
organs the results for second and subsequent trans- plants are inferior to
first transplants. For kidney, pancreas and liver there must be an expectation
that the recipient will survive 5 years after the operation. UK listing
criteria are given below.
Kidney transplantation
Already on, or estimated to be within 6 months of starting
dialysis (e.g. using a reciprocal creatinine graph). Re-transplantation is permitted providing it is surgically
feasible and the patient is fit; the main limiting factor is sensitisation
against HLA antigens.
Pancreas transplantation
1. Combined
(simultaneous) pancreas and kidney (SPK) transplantation:
GFR ≤ 20 ml/min or on dialysis and type 1 diabetes (or type 2 if BMI
<30 kg/m2).
2. Pancreas
or islet transplantation alone (PTA/ITA): life-threatening
hypoglycaemic unawareness.
3. Pancreas
after kidney transplantation (PAK): severe diabetic complications and
satisfactory function of prior renal transplant, since function is affected by
increased doses of nephrotoxic immunosuppression.
Liver transplantation
There is no bar on re-transplantation, but since results of retransplants
are so much poorer, the patient should be otherwise in good health. Individual
criteria exist for subgroups, such as hepatocellular tumours or acute liver
failure (see Chapter 33).
Heart transplantation
Patients are accepted according to internationally agreed
criteria. Many patients are now supported by mechanical devices, and are
regarded as stable on the waiting list. They only receive priority if they
develop complications such as drive-line infections. Re-trans- plants can be
done with reasonably good outcomes, but not in the first 3 months after the
initial procedure.
Lung transplantation
Most patients are now listed for bilateral lung transplants. The
only group regularly receiving single lungs are those with fibrotic disease,
where the shrunken chest cavity cannot easily accept a pair of lungs.
Re-transplants are done with increasing frequency, although still
amount to only 5–6% of activity.
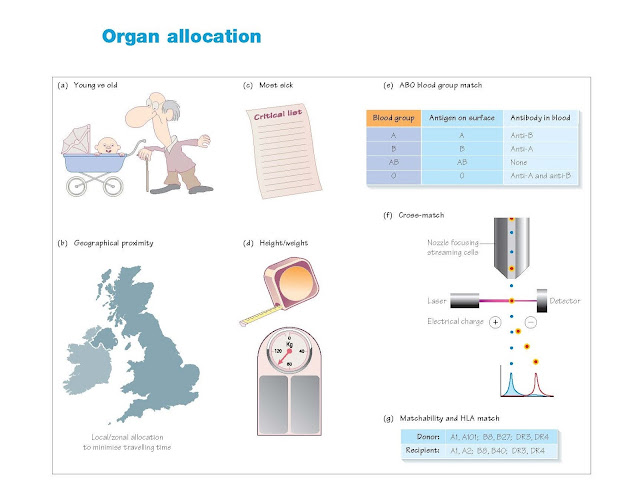
Principles in organ allocation
Organ allocation is an exercise in distributive justice, how to
fairly divide up a limited resource. There are several criteria that may be
used for organ allocation.
Equity (fairness): everyone
should have equal access to organs. Such a scheme would allocate organs first
to those who have been waiting longest, and to young and old alike.
Utility: organs should be allocated to achieve
the greatest number of life-years following transplantation, independent of
other factors. For example, since outcomes of kidney transplantation are poorer
in those already on dialysis and in the elderly, these two groups would be
excluded in a utilitarian allocation scheme, in direct contrast to the
egalitarian approach.
Greatest need: the organ goes to the person whose
medical condition demands it the most.
Greatest benefit: organs are
allocated to achieve the greatest benefit, in terms of life-years gained,
compared with remaining on the waiting list. Such allocation acknowledges that
organs are different, with young donor organs having a better anticipated longevity
than older organs. Thus an old donor kidney may be best allocated to an older
recipient, who has a high mortality on dialysis and for whom an old kidney
would increase their survival significantly. A young recipient has a better
survival on dialysis so there is less gain from having an old kidney, which
would last only a short time period.
Allocation in practice
In reality, current allocation schemes involve a mixture of the
above principles. Organs are allocated to ABO-identical recipients, with the
exception of group A organs, which may go to AB recipients, and occasional
group O organs, which may go to group B (or A or AB) recipients in special
circumstances (e.g. medical urgency or HLA sensitisation).
Organs are transplanted to avoid pre-existing donor-specific HLA
antibodies (a positive cross-match), with the exception of the liver, which can
be transplanted into a recipient who possesses antibodies to the donor’s MHC
class 1 antigens.
Kidney
Kidneys are allocated primarily to HLA-matched recipients, prioritising
sensitised patients over non-sensitised, children over
adults. Thereafter allocation is according to a complex formula
that assigns points for:
· HLA
mismatch, aiming to optimise matching
· time
on the waiting list, prioritising long waiters
· sensitisation
(HLA antibodies) and matchibility (unusual HLA type), giving priority to
patients who are hardest to find a compatible transplant
· HLA-B
and -DR homozygous recipients, correcting an imbalance that prioritising
according to HLA mismatch creates
· age
difference, aiming to minimise age difference between donor and recipient.
In addition children (under 18) get priority over adults.
Pancreas for islets or whole organ
An algorithm assigns points for:
· HLA
mismatch, aiming to optimise matching
· HLA
sensitisation and matchibility
· waiting
time, giving additional priority to an islet recipient awaiting a second graft
and a pancreas recipient on dialysis
· distance
of donor to recipient centre, to minimise ischaemic time.
Liver
Livers are allocated within seven zones in the UK corresponding to
each liver transplant unit. Priority is given to the sickest patient (UKELD
score, see Chapter 33) of a compatible size – big livers don’t fit small
abdomens.
A ‘super-urgent’ scheme exists for anyone with acute liver failure
with an expected of survival of less than 3 days; a third of these patients die
while waiting and outcomes are poorer than for chronic liver disease.
Heart
Like livers, hearts and lungs are allocated within zones corresponding
to each of the six transplant centres. Matching is done by blood group and size
of donor, which needs to be within 10% of that of the recipient. Female hearts
placed in male recipients do measurably less well, and this combination is
avoided.
There is also an urgent scheme for hearts, which accounts for
nearly half of all transplants performed. The results are at least as good as
those for ‘elective’ patients. These recipients have the most to gain from
transplantation.
Lung
Size is of great importance in lung allocation–large lungs do
not fit into small recipients. If small lungs are placed in a large chest they
become over-inflated. Allocation is done as for hearts and livers, on a local
basis, but there is no urgent system. Individual centres identify the sickest
patients on their waiting list. A lung that cannot be used locally is offered
nationally around the other centres.
Intestine
Intestinal donors are offered as a priority to the four intestinal
transplant centres (two adult, two child). For most intestinal transplants size
is the critical factor, with only the smaller donors (below 50 kg) being suitable.