Benign And Malignant
Diseases Of The Breast
Breast
complaints are common in women and most diseases of the breast (96%) are
nonmalignant. Histologic subcategorization of breast masses, based upon
cellular proliferation and the presence or absence of hyperplasia, divides
these lesions into three subgroups. Nonproliferative lesions include
simple and complex cysts. While most cystic lesions do not increase breast
cancer risk, complex cysts containing solid and cystic components on ultrasound
have increased malignant potential. Proliferative lesions without atypia include
fibroadenomas, simple ductal and intraductal hyperplasia, sclerosing adenosis
and papillomas. The latter are often associated with unilateral nipple
discharge. All of these solid lesions increase breast cancer risk with a
relative risk (RR) of 1.6–1.9. Proliferative lesions with atypia (atypical
hyperplasia) can be of ductal or lobular origin. They increase the risk of
breast cancer 3.7–5.3-fold.
Other common
breast disorders include mastitis, cyclical breast pain and nipple discharge.
Mastitis affects 3–10% of lactating women and typically presents as unilateral
breast pain and high fever. Cyclical breast pain is often related to the
hormonal changes of the menstrual cycle. Risk of malignancy after normal exam
and imaging of the painful breast is very low. Most women of reproductive age
can express discharge from their nipples. However, unilateral discharge, the
presence of blood, age greater than 40 and association with a breast mass are concerning
and require additional testing.
Breast cancer
Breast
cancer is the most common malignancy in women. In addition to occuring almost
exclusively in women, it is also a disease of aging. The lifetime risk of
developing breast cancer (1 in 8) is largely concentrated in the perimenopausal
and postmenopausal years. Risk in the 30-year-old is 1 in 2525, that in a
45-year-old 1 in 93 and that in a 65-year-old 1 in 17. Older women tend to
underestimate their risk and many women under 50 years of age grossly
overestimate their risk. Consequently, these two groups of women misjudge the
benefits of breast cancer screening programs.
Breast
cancer can arise anywhere in the mammary gland. Tumors are typically classified
by their cells of origin: lobular or ductal. Ductal carcinomas account for 85%
of breast cancers and can be either non-invasive (intraductal) or
infiltrating. Those ductal carcinomas that are histologically confined by the
basement membrane of the duct are called intraductal carcinomas or ductal
carcinoma in situ (DCIS). DCIS is considered a precursor lesion to
invasive carcinoma. At least 33% of these lesions will progress to invasive
cancer within 5 years. Once the basement membrane of the duct is breached, an
infiltrating carcinoma has developed. The most common type of invasive carcinoma is ductal carcinoma, which accounts for 79% of invasive carcinomas. The
next most common type is lobular carcinoma. These lesions arise from the
terminal ductules of the alveoli and comprise approximately 10% of invasive
breast cancers. Less common types of infiltrating carcinomas include
medullary carcinomas, mucinous (colloid) carcinomas and Paget disease. Paget
disease is a special subtype of infiltrating ductal carcinoma localized to a
main lactiferous duct. In Paget disease, eczematous changes develop in the
nipple and areola overlying the affected duct. These skin changes are often the
first sign of disease although the cancer may have been present for some time.
Breast
cancer metastasizes first to the regional axillary lymph nodes. The most
frequent distant metastatic sites are bone, liver, lung, pleura and brain.
Patients with histologically negative axillary nodes have a much higher
likelihood of survival than do patients with positive nodes. The ultimate
prognosis for the disease depends on the size of the tumor, the number of
involved lymph nodes and whether or not lymphovascular invasion (LVI) is
present.
Treatment of
invasive breast cancer is typically multimodal, but ultimately depends on the
stage of the disease at the time of diagnosis. Surgical options include a
modified radical mastectomy or lumpectomy with local irradiation. Ipsilateral
axillary lymph node dissection is also typically performed. Women with positive
lymph nodes will usually receive additional antineoplastic chemotherapy. Those
with negative nodes will receive adjuvant chemotherapy if they have large primary
tumors or LVI, because both confer a high risk of tumor recurrence. Tamoxifen
is a medication with estrogenic and antiestrogenic properties; it is the most
widely used endocrine therapy for breast cancer. Before employing endocrine
therapy, it is important to know the estrogen and progesterone receptor status
of the tumor because only receptor-positive tumors predictably respond to
medications like tamoxifen.
Treatment of
DCIS is controversial and includes mastectomy or wide local excision plus
irradiation. Recurrence rates following excision plus radiation are
approximately 10%; half of these are invasive.
Epidemiology of breast cancer
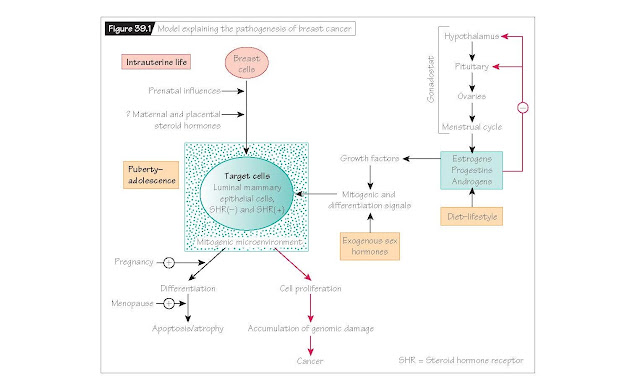
The
epidemiology of breast cancer in women suggests that it is an endocrine
disorder related to prolonged exposure to ovarian hormones (Fig. 39.1). Ovarian
hormones have been shown to increase the mitotic activity of mammary cells in
culture. In addition to the factors listed in Table 39.1, hormonal treatment in the form of
postmenopausal hormone replacement therapy may contribute to a higher lifetime
risk of breast cancer.
There are
also large ethnic and geographic differences in the prevalence of breast
cancer. Asian women born and raised in Asia have one-fifth the risk of
developing breast cancer that American women have. The risk rises toward the
American level if Asians live in the USA for two or more generations,
suggesting an environmental or lifestyle influence on the disease. Even within
a single large country, breast cancer incidence and mortality rates can vary by
location. In more affluent areas, breast cancer rates are elevated. This may be
related to delayed child-bearing among more affluent and better educated women.
The association of alcohol intake with increased breast cancer risk suggests
there is an environmental influence on its development.
Familial breast cancer
About 10% of
breast cancer is familial. The clustering of breast cancers with ovarian
cancers in many familial cases led to the discovery of two genes, BRCA1 and
BRCA2. Individuals with germline mutations in these genes are at high
risk for the development of specific cancers. Current evidence indicates that
25% of inherited cases of breast cancer result from mutations involving BRCA1
and BRCA2. Both BRCA1 and BRCA2 are tumor suppressor
genes and mutation in a single allele of either gene confers an increased
cancer risk. The ethnic and geographic distributions of BRCA1 and BRCA2
are discussed in more detail in Chapter 42.
Molecular biology of sporadic
(nonfamilial) breast cancer
Molecular
studies have identified several genetic loci that are frequently abnormal in
breast cancer specimens but not in normal breast tissues. The most commonly
encountered abnormalities involve the oncogenes, ERBB2 and c-myc,
the tumor suppressor gene TP53, and telomerase. Both oncogenes are
amplified or overexpressed in about 30% of breast cancers; telomerase activity
is elevated in 80–90%. Breast tissue with ERBB2 abnormalities appears to
be resistant to the effects of the antiestrogen tamoxifen but more sensitive to
standard chemotherapeutic agents. TP53 abnormalities interfere with
normal apoptosis, thereby making affected tumors more resistant to chemotherapy
and radiation therapy. Like most malignancies, breast cancer probably results
from the effects of environmental triggers on genetically susceptible tissues.