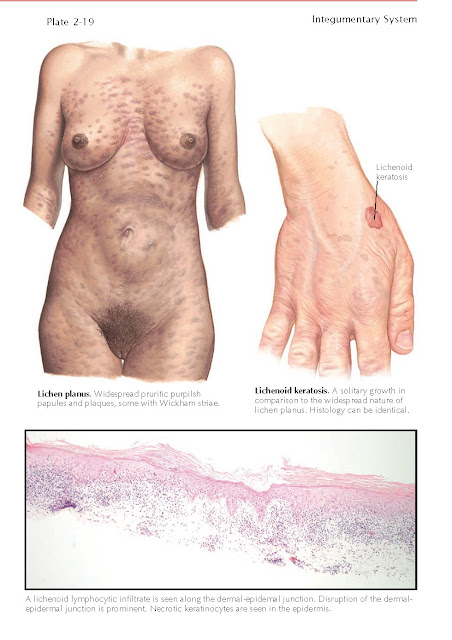
LICHENOID KERATOSIS
Lichenoid
keratoses are common benign skin growths also known as lichen planus like
keratoses. These are most often solitary, benign skin tumors and may be found
anywhere on human skin. They are more common during adulthood. The keratosis
may be misdiagnosed as a non-melanoma skin cancer, most commonly a superficial
basal cell carcinoma.
Clinical Findings: Lichenoid keratoses are most frequently found on
the upper trunk and upper extremities. The incidence is equal in males and
females, and there is no race predilection. They are rare in childhood. They
typically manifest as pruritic, red to slightly purple patches and thin
plaques. Occasionally, a patient notices that the area arises in a preexisting
seborrheic keratosis or solar lentigo. Most lichenoid keratoses are 1 cm or
smaller in their largest diameter. Most patients present to their physician
with a chief complaint of tenderness, itching, or bleeding secondary to
scratching or rubbing of the lesion. The lesions may have a striking
resemblance to the rash of lichen planus; the differentiating factor is that a
lichenoid keratosis is solitary, whereas lichen planus includes a multitude of
similar skin lesions. These skin growths have no malignant potential. It can be
difficult to differentiate lichenoid keratoses from inflamed seborrheic
keratoses, basal cell carcinomas, actinic keratoses, or squamous cell carcino-
mas. Therefore, a biopsy of the lesion is prudent to discern a pathological
diagnosis.
There are a few unusual clinical
variants, including an atrophic form and a bullous type of lichenoid keratosis.
The differential diagnosis of these two variants includes conditions such as
lichen sclerosis for the former and autoimmune blistering diseases for the
latter. The dermatoscope has become an indispensable tool and can be helpful in
diagnosing lichenoid keratosis. Lichenoid keratoses have been shown to have a
localized or diffuse granular-type pattern under dermatoscopic viewing. This
finding should help differentiate these tumors from melanocytic tumors.
Histology: On histological examination, a lichenoid keratosis
has a symmetric, well-circumscribed area of intense lichenoid inflammation
along the basement membrane region. There is disruption of the basilar
keratinocytes. This leads to the appearance of a number of necrotic
keratinocytes, also called Civatte bodies. Civatte bodies are seen in almost
all cases of lichenoid keratosis and also in lichen planus. There is pronounced
sawtooth hypergranulosis and pronounced acanthosis. There is no atypia of the
involved keratinocytes, thus ruling out an inflamed actinic keratosis. The
underlying inflammatory infiltrate is made up almost entirely of lymphocytes.
However, it is not uncommon to find a rare eosinophil or plasma cell anywhere
throughout the infiltrate. The pathological differential diagnosis includes
lichen planus. The clinical history is very important: Whereas a lichenoid
keratosis is a solitary lesion, the same findings in a biopsy specimen taken
from a widespread rash of purple, flat-topped papules would be more consistent
with the diagnosis of lichen planus. This example illustrates the importance of
including the clinical history on a pathology report.
Pathogenesis: The exact etiology of a lichenoid keratosis is
unknown. It is believed to be caused by an inflammatory response to a lentigo
or a thin seborrheic keratosis. The specific precipitating factor may be
trauma. Chronic rubbing has been implicated in inducing lichenoid keratoses
from lentigines. The role of human papillomavirus (HPV) in causing lichenoid
keratoses has been studied, but no firm conclusions have been made.
Treatment: Most biopsies of a lichenoid keratosis result in
complete resolution of the lesion. Even if the entire lesion was not removed
with the biopsy specimen, no treatment is necessary. Use of a topical
corticosteroid cream or ointment twice daily for 1 to 2 weeks after healing of
the biopsy site is likely to lead to complete resolution of the lichenoid
keratosis. Other treatment options include light cryotherapy or a light
curettage after anesthesia. Benign lichenoid keratoses rarely if ever recur.