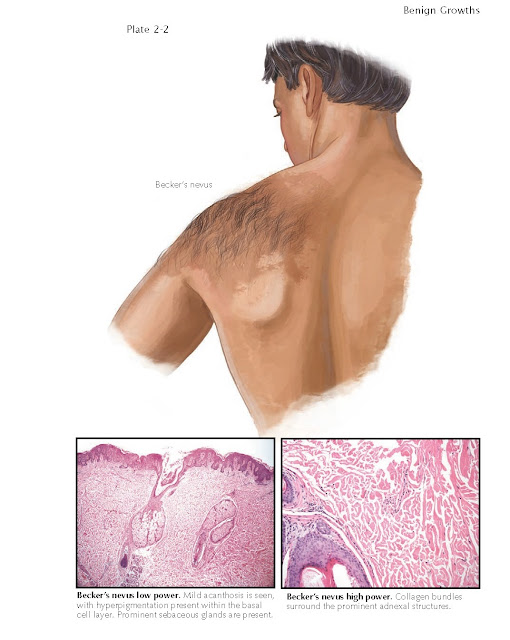
BECKER’S NEVUS (SMOOTH MUSCLE HAMARTOMA)
Becker’s nevi most
commonly appear on the shoulder or upper limb girdle of prepubescent boys. It
is a rather common benign condition that is seen in up to 0.5% of the male
population. It is less commonly seen in females. Becker’s nevi are acquired
nevi. Most occur before 10 years of age. Becker’s nevus is classified as a
smooth muscle hamartoma. It does not contain melanocytic nevus cells and is not
considered to be a melanocytic nevus. It was given its name by the
dermatologist Samuel Becker, who first described this condition.
Clinical Findings: Becker’s nevi begin as ill-defined,
slightly hyperpigmented macules on the upper limb girdle. Over time (1 year, on
average), the hyperpigmented region develops hypertrichosis, resulting in its
characteristic appearance. Backer’s nevi may occur anywhere on the human body,
but by far the most common locations are on the shoulder, upper chest, and
back. The area of hypertrichosis is limited to the underlying hyperpigmented
area. The clinical significance of Becker’s nevi is its differentiation from
large congenital nevi and café-au-lait macules. Becker’s nevi confer no
increased risk for development of melanoma, and they are rarely associated with
any underlying abnormalities. The most common underlying abnormality is
unilateral hypoplasia of the breast, which has minimal clinical significance.
Rarely, a patient with a Becker’s nevus has underlying hypoplasia of bone and soft
tissue, the cause of which is unknown. The differential diagnosis includes a
giant congenital nevus and a café-aulait macule. These two conditions should be
easily differentiated from Baker’s nevus, because they both are typically
apparent at birth or soon there- after, whereas Becker’s nevi are typically
acquired at about the age of 10 years.
The diagnosis is typically made on clinical findings, but a skin biopsy
is sometime needed to confirm the diagnosis if the nevus is in an unusual
anatomical location. The punch biopsy is the best method for obtaining tissue.
Histology: The biopsy specimen shows a smooth muscle
hamartoma. Multiple smooth muscle fascicles are seen within the dermis. There
is an increased ratio of terminal to vellus hairs and a lack of melanocytic
nevus cells. The hyperpigmentation results from increased formation of
pigmentation within the melanocytes of the stratum basalis. There is no
increase in the number of melanocytes. Varying amounts of acanthosis and
hyperkeratosis are seen.
Pathogenesis: The pathogenesis of Becker’s nevus is
unclear. It is believed to be caused by the dermal presence of hamartomatous
smooth muscle tissue. Research has shown that the tissue in Becker’s nevi has
an increased number of androgen receptors. It is thought that increased
androgen levels at puberty interact with the excessive androgen receptors and
cause the clinical findings.
Becker’s nevus is the most common type of smooth muscle hamartoma in the
skin. Smooth muscle hamartomas by themselves are rarely found within the skin.
Non-Becker’s smooth muscle hamartomas are usually present at birth or
soon thereafter and manifest as a small, flesh-colored plaque located anywhere
on the body. All smooth muscle hamartomas may at some point exhibit the
pseudo-Darier’s sign. To clinically elicit this sign, one gently rubs the smooth
muscle hamartoma; the lesion may fasciculate due to smooth muscle activity, or
the region may develop an urticarial appearance. This sign has nothing to do
with histamine release; rather, it is
caused by a neurally mediated con- traction of the underlying hamartomatous
smooth muscle tissue.
Treatment: No therapy is required. Surgical excision is
likely to produce a mutilating scar unless the nevus is extraordinarily small.
The hypertrichosis can be treated for cosmetic purposes with any of a multitude
of therapies including laser removal, shaving, and electrolysis. Most patients
prefer to not treat the area.