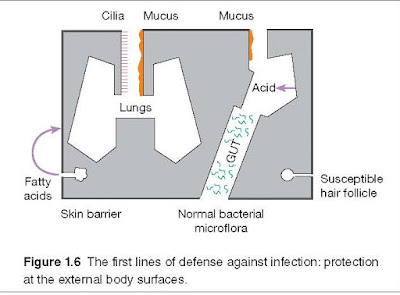
External Barriers Against Infection
As mentioned above, the simplest
way to avoid infection is to prevent the microorganisms from gaining access to
the body (Figure 1.6). When intact, the skin is impermeable to most infectious
agents; when there is skin loss, as for example in burns, infection becomes a
major problem. Additionally, most bacteria fail to survive for long on the skin
because of the direct inhibitory effects of lactic acid and fatty acids in
sweat and sebaceous secretions and the low pH that they generate. An exception
is Staphylococcus aureus, which often infects the relatively vulnerable
hair follicles and glands.
Mucus, secreted by the membranes
lining the inner surfaces of the body, acts as a protective barrier to block
the adherence of bacteria to epithelial cells. Microbial and other foreign
particles trapped within the adhesive mucus are removed by mechanical
stratagems such as ciliary movement, coughing, and sneezing. Among other mechanical
factors that help protect the epithelial surfaces, one should also include the
washing action of tears, saliva, and urine. Many of the secreted body fluids
contain bactericidal components, such as acid in gastric juice, spermine and
zinc in semen, lactoperoxidase in milk, and lysozyme in tears, nasal
secretions, and saliva.
A totally different mechanism is
that of microbial antagonism associated with the normal bacterial
flora of the body (i.e., commensal bacteria). This suppresses the growth of
many potentially pathogenic bacteria and fungi at superficial sites by
competition for essential nutrients or by production of inhibitory substances.
To give one example, pathogen invasion is limited by lactic acid produced by
particular species of commensal bacteria that metabolize glycogen secreted by
the vaginal epithelium. When protective commensals are disturbed by
antibiotics, susceptibility to opportunistic infections by Candida and Clostridium
difficile is increased. Gut commensals may also produce colicins, a class
of bactericidins that bind to the negatively charged surface of susceptible
bacteria and insert a hydrophobic helical hairpin into the membrane; the
molecule then undergoes a “Jekyll and Hyde” transformation to become completely
hydrophobic and forms a voltage‐dependent channel in the membrane that kills
by destroying the cell’s energy potential. Even at this level, survival is a
tough game.
If microorganisms do penetrate
the body, the innate immune system comes into play. Innate immunity involves
two main defensive strategies to deal with a nascent infection: the destructive
effect of soluble factors such as bactericidal enzymes and the
mechanism of phagocytosis – literally “eating” by the cell (see
Milestone 1.1). Before we discuss these strategies in more detail, let us first
consider the major cellular players in the immune system.