Deceased
Organ Donation
Opting in or opting out?
In the UK, as in most countries in the world, the next of kin are
approached for consent/authorisation for organ donation, a system known
colloquially as ‘opting in’. This system is facilitated by having a register,
such as the UK organ donor register (ODR), where people can register their
wishes to be a donor when they die; 29% of the UK population are on the
register. However, opinion polls show that nearer to 90% of people are in
favour of organ donation, suggesting that the shortfall is a consequence of
apathy. When a person is on the ODR the relatives are much more likely (>90%)
to consent to donation than where the wishes of the deceased were not known (∼60%).
In some parts of the world, most notably Spain, a system of presumed
consent exists where you are presumed to have wanted to be an organ donor
unless you registered your wish in life not to be so, i.e. you ‘opted out’.
Spain also has the highest donation rate in the world, so on the face of it a
switch to opting in should improve donation. However, there are other points to
consider.
· Spain
had presumed consent for 10 years before its donation rate rose – only after
reorganising the transplant coordination infra- structure did donation rates
rise, and it has been argued that it was this, not presumed consent, that was
the key factor.
· Even
in Spain, the relatives are asked for permission and their wishes observed.
· Other
reasons that Spain has a higher donation rate than the UK include using organs
from a wider age range, with many more donors over 60 and 70 being used than in
the UK.
· Some
countries with presumed consent, such as Sweden, have donation rates below that
of the UK.
Patterns of organ donation
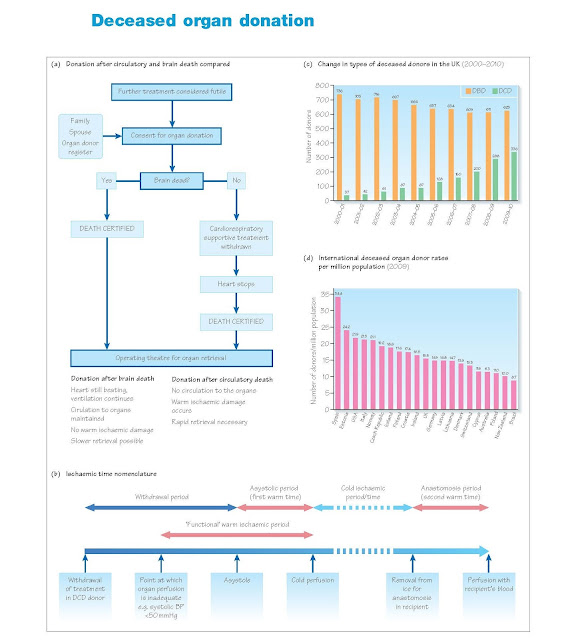
The past decade has seen an increase in the number of deceased organ
donors in the UK. That increase has been due to a 10-fold increase in DCD
donors, who now comprise a third of all deceased donors in the UK. The number
of donation after brain death (DBD) donors has fallen, although the proportion
of potential DBD donors for whom consent for donation is obtained has
increased.
Organ retrieval
DBD donation
Since DBD donors are certified dead while on cardiorespiratory support,
the organs continue to be perfused with oxygenated blood while the retrieval
surgery takes place. Once the dissection phase is completed, ice-cold
preservation solution is passed through a cannula into the aorta with
exsanguination via the vena cava; at the same time ice-cold cardioplegia is
perfused into the coronary arteries to arrest the heart. The organs are flushed
and cooled in situ, removed and then placed into more preservation solution and
packaged for transit in crushed ice.
DCD donation
In contrast to DBD donation, the circulation has, by definition, already
ceased in DCD donors before organ retrieval commences. In controlled DCD
donation, the surgical team is ready and waiting in the theatre, while
treatment is withdrawn either in the ITU or in the theatre complex. Death may
then be instantaneous, but more
commonly follows a variable period of time while the blood pressure falls
before cardiac arrest occurs. When the blood pressure is insufficient to
perfuse the vital organs, functional warm ischaemia commences. In the UK no
treatment can be given to the donor prior to death; in the US it is permissible
to give heparin to prevent in situ thrombosis. When the retrieval surgery
begins the organs are still warm and already ischaemic. Unlike DBD donation,
where the organs are mobilised while a circulation is still present, for DCD
donation the abdominal organs are perfused with cold preservation solution as
soon as the abdomen is opened, to convert warm ischaemia to cold ischaemia;
once cooled the organs are rapidly mobilised and removed.
Ischaemic times
The nomenclature used for the time periods from donation to
transplantation is shown in Figure 3c. Warm ischaemia is most deleterious to an
organ, and it is often said that a minute of warm ischaemia does the same
damage as an hour of cold ischaemia. Since the duration of ischaemia is one of
the few things that a surgeon can modify to improve the outcome following
transplantation, every effort is made to minimise both warm and cold ischaemia
and to transplant the organs as soon as possible.
Contraindications to donation
It has long been established that malignancy and infection can be
transferred with a donor organ to the recipient. However, there are occasions,
such as when a potential recipient will die if not transplanted immediately,
where the balance of risks may favour using at-risk organs. Nevertheless the
following are generally considered contraindications to donation:
· Active
cancer, except skin cancer (not melanoma) and some primary brain tumours; this
includes recently treated cancers;
· Untreated
systemic infection;
· Hepatitis
b or c or hiv, except to similarly infected recipients;
· Other
rare viral infections, e.g. Rabies.
At the time of retrieval the donor surgeon must do a thorough laparotomy
and thoracotomy looking for evidence of occult malignancy, such as a lung,
stomach, oesophageal or pancreatic tumour. In addition, it goes without saying
that evidence of severe, permanent damage to the organ to be transplanted is a
contraindication to its use, e.g. a heart with coronary artery disease or a
cirrhotic liver.
Suboptimal organs
Less than ideal organs, sometimes called expanded criteria or marginal
organs, are those whose anticipated function is likely to be less than ideal,
but nevertheless adequate. Every recipient would like a new organ, but the
reality is that all organs are ‘second hand’, and someone dying below the age
of 60 usually has significant other comorbidity that contributed to their early
death, such as cigarette smoking-associated pathologies or hyper- tension.
Deaths from trauma are increasingly uncommon. The severe shortage of organs,
particularly from young donors, means that compromises have to be made to
balance the risks of dying on the waiting list: 25% of patients awaiting a lung
transplant will die in the first year of waiting, as will 15% of those awaiting a liver.