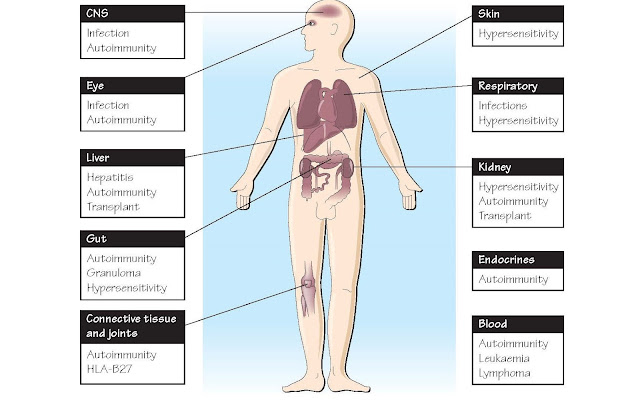
Immunity And Clinical Medicine
Clinical immunology is a specialty in its own right and there are many
excellent textbooks devoted to it. Here
we can only summarize the most common conditions encountered by the clinical
immunologist, arranged by organs and/or systems rather than, as
elsewhere in this book, by mechanism. Obviously there are frequent
overlaps with other disciplines, which is why the clinical immunologist is
expected to be familiar with all branches of pathology and medicine. For
example, a case of myeloma could present to the accident and emergency department
(A&E) with a fracture or be referred to the rheumatology department because
of bone pain, to urology because of renal failure, to haematology because of anaemia, to immunology because
of immunodeficiency, or even to the
neurology or eye clinic. Abnormalities may be picked up by the radiologist, by
the haematologist in a marrow biopsy, or simply from serum electrophoresis or a
urine test. In the same way any patient with liver, kidney, lung, joint or skin
disease, or with an unusual infection, should be looked at with the
immunological possibilities in mind. The figure can be used as a checklist;
brief details are provided on the opposite page. Remember that immune status is
critical when considering vaccination, transplantation and in monitoring the course
of AIDS.
CNS Blood–brain barrier keeps out most infections.
1 Meningitis: usually bacterial; encephalitis
more often viral (NB prions: Creutzfeldt–Jakob disease [CJD]).
2 Multiple sclerosis: plaques of demyelination in
brain, with Ig in cerebrospinal fluid (CSF); progressive with remissions, IFNβ
delays progression.
3 Guillain–Barré syndrome: demyelination in
peripheral nerve post infection; normally complete recovery.
4 Myasthenia gravis: autoimmune destruction of
acetylcholine recep- tors at nerve–muscle junction; muscle fatigue; maternal
antibody can affect neonate; plasmapheresis to remove antibody.
Eye The eye, open to the air, is protected from
infection by tears, lysozyme and IgA.
5 Common infections: adenovirus, Streptococcus
pneumoniae (con- junctiva), trachoma (eyelid), CMV, Toxoplasma spp.
(retina), congeni- tal rubella (lens).
6 Uveitis: common in rheumatic and other systemic
autoimmune diseases.
7 Sympathetic ophthalmia after unilateral damage.
8 Corneal grafts: 65% non-rejection.
Liver
• Hepatitis
B and C: damage to liver cells by chronic cytotoxic T-cell activation, not by
virus; 10% (B) and 50% (C) become
carriers. Persistent ‘chronic active’ disease, may lead to cirrhosis, carcinoma. Congenital adrenal hyperplasia
(CAH) may also be autoimmune, Wilson’s disease (copper), haemochromatosis (iron). Hepatitis A and B
vaccines available.
• Primary
biliary cirrhosis: autoimmune, with antimitochondrial anti- bodies; probably
bacterial cross-reaction.
• Possibility
of transplant for liver failure.
Gut
• Sjögren’s syndrome:
salivary gland autoimmunity; dry mouth.
• Pernicious
anaemia: autoimmune gastritis plus antibody to intrinsic factor; vitamin B12
not absorbed.
• Coeliac
disease: α-gliadin hypersensitivity leading to jejunal malabsorption.
Controlled by gluten-free diet.
• Crohn’s
disease: constricting granulomas in small intestine. May result from granulocyte
functional deficit.
• Ulcerative
colitis: ulcers may bleed. Both ulcerative colitis and Crohn’s disease show lymphocytic
infiltration.
Connective tissue and joints
• Rheumatoid
arthritis: IgM antibodies to IgG (rheumatoid factor [RF]) in 70%, suggestive
but not diagnostic. No infectious cause identified. May be changes in lung,
skin, blood vessels, etc. T cells, plasma cells, macro- phages, cytokines in
joints. Blocking TNF effective.
• Seronegative
arthritis (i.e. no RF): includes ankylosing spondylitis (90 times greater risk
if HLA-B27) and Reiter’s disease (post bowel or genitourinary infection –
‘reactive’ arthritis).
• Systemic
lupus erythematosus: multiorgan pathology (lung, kidney, skin rash, brain);
antibodies to nuclei (ANA), dsDNA, 25%
have RF. High circulating interferon levels. Some cases due to drugs.
• Systemic
sclerosis: multiorgan, may have RF, ANA, CREST syndrome (calcinosis, Raynaud’s,
oesophageal dysmotility, sclerodactyly, telangiectasia).
• Polymyositis:
muscle and joint lesions.
• Dermatomyositis:
muscle, joints, skin.