Agents of Infectious
Disease
The
agents of infectious disease include prions, viruses, bacteria, Rickettsiaceae
and Chlamydiaceae, fungi, and parasites. A summary of the salient
characteristics of these human microbial pathogens is presented in Table 12.2.
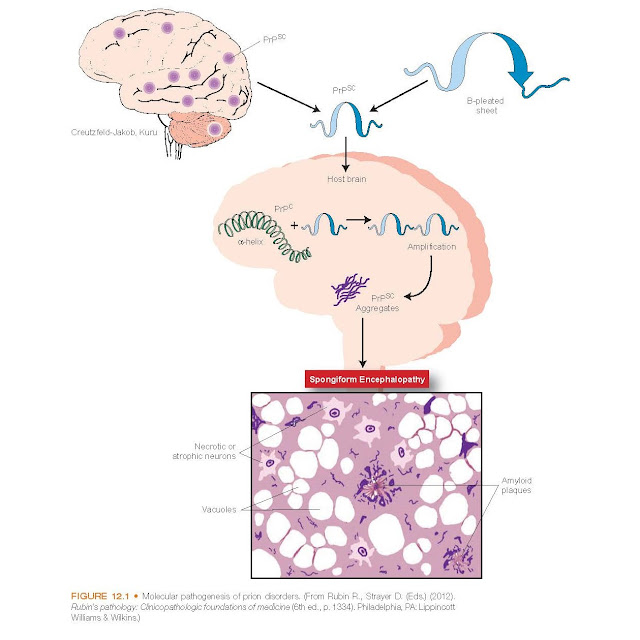
Prions
In the
past, microbiologists have assumed that all infectious agents must
possess a genetic master plan (a genome of either ribonucleic acid [RNA] or
deoxyribonucleic acid [DNA]) that codes for the production of the essential
proteins and enzymes necessary for survival and reproduction. However, it is
now known that infection can be transmitted solely by proteins and no nucleic
acid. Prions, protein particles that lack any kind of a demonstrable genome,
are able to transmit infection. A number of prion-associated diseases have been
identified, including Creutzfeldt-Jakob disease and kuru in humans, scrapie in
sheep, chronic wasting disease in deer and elk, and bovine spongiform
encephalopathy (BSE or mad cow disease) in cattle. The various prion-associated
diseases produce very similar pathologic processes and symptoms in the hosts
and are collectively called transmissible neurodegenerative diseases (see
Fig. 12.1). All are characterized by a slowly progressive, noninflammatory
neuronal degeneration, leading to loss of coordination (ataxia), dementia, and
death over a period ranging from months to years. In fact, evidence indicates
that scrapie prion proteins (called PrPSC) are actually altered or mutated
forms of a normal host protein called cellular PrPC. Differences in the
posttranslational structure cause the two proteins to behave differently. The
PrPSC is resistant to the action of proteases (enzymes that degrade excess or
deformed proteins) and aggregates in the cytoplasm of affected neurons as
amyloid fibrils. The normal PrPC is protease sensitive and appears
on the cell surface.
Prion
diseases present significant challenges for management due to the pathogenic
structure of PrPSC. It is very stable
and, therefore, is resistant to many antibiotics. Studies investigating transmission of prion diseases in
animals clearly demonstrate that prions replicate, leading researchers to investigate
how proteins can reproduce in the absence of genetic material. Based on current
models, it is believed that PrPSC binds to the normal PrPC
on the cell surface, causing it to be processed into PrPSC, which is
released from the cell and then aggregates into amyloid-like plaques in the
brain. The cell then replenishes the PrPC and the cycle continues.
As PrPSC accumulates, it spreads within the axons of the nerve
cells, causing progressively greater damage of host neurons and the eventual
incapacitation of the host. Prions lack reproductive and metabolic functions,
so the currently available antimicro- bial agents are useless against them.
Viruses
Viruses
are the smallest obligate intracellular pathogens. They have no organized
cellular structures but instead consist of a protein coat, or capsid,
surrounding a nucleic acid core, or genome, of RNA or DNA never both
(Fig. 12.2). Some viruses are enclosed within a lipoprotein envelope derived
from the cytoplasmic membrane of the parasitized host cell. Enveloped viruses
include members of the herpesvirus group and paramyxoviruses (e.g.,
influenza and poxviruses). Certain enveloped viruses are continuously shed from
the infected cell surface enveloped in buds pinched from the cell membrane.
The
viruses of humans and animals have been categorized somewhat arbitrarily
according to various characteristics. These include the type of viral genome
(single-stranded or double-stranded DNA or RNA), physical characteristics (e.g.,
size, presence or absence of a membrane envelope), the mechanism of
replication (e.g., retroviruses), the mode of transmission (e.g., arthropod-borne
viruses, enteroviruses), target tissue, and the type of disease produced (e.g.,
hepatitis A, B, C, D, and E viruses), to name just a few.
Viruses
are incapable of replication outside of a living cell.
They must penetrate a susceptible living cell and use the biosynthetic structure of the cell to produce viral
progeny.
The
process of viral replication is shown in Figure 12.3. Not every viral agent
causes lysis and death of the host cell during the course of replication. Some
viruses enter the host cell and insert their genome into the host cell
chromosome, where it remains in a latent, nonreplicating state for long periods
without causing disease. Under the appropriate stimulation, the virus undergoes
active replication and produces symptoms of disease
months to years later. Members of the herpesvirus group and adenovirus are
examples of latent viruses. Herpesviruses include the viral agents of chicken-
pox and zoster (varicella–zoster), cold sores (herpes simplex virus [HSV] type
1), genital herpes (HSV type 2), cytomegalovirus infections, roseola (human
herpesvirus 6), infectious mononucleosis (IM)
(Epstein-Barr virus [EBV])
(see Fig. 12.4), and
Kaposi sarcoma (herpesvirus 8). The resumption of the latent viral replication
may produce symptoms of primary disease (e.g., genital herpes) or cause
an entirely different symptomatology (e.g., shingles instead of
chickenpox).
A family
of viruses that has gained a great deal of attention is the Orthomyxoviridae or
flu viruses. There has been attention focused on the H5N1 variant, commonly
known as the avian influenza virus, and the H1N1 variant, commonly known
as swine flu. The avian influenza viruses differ from the usual human
influenza viruses by the hosts they normally infect.
Avian
influenza viruses typically infect wild birds. However, on occasion a new virus may result from genetic
rearrangements that make it better fit to infect humans. When this occurs, the
human population is more susceptible because the virus is unfamiliar to most of
our immune systems. The H1N1 or swine flu was most notable in 2009. This influenza
A virus was susceptible to oseltamivir (Tamiflu), but resistant to amantadine.
Rapid influenza diagnostic tests (RITs) have been developed to diagnose a
person with H1N1 and other influenza viruses.
Since the
early 1980s, members of the retrovirus group have received considerable
attention after identification of the human immunodeficiency viruses (HIV) as
the causative agent of acquired immunodeficiency syndrome (AIDS). The retro-viruses
have a unique mechanism of replication. After entry into the host cell, the
viral RNA genome is first translated into DNA by a viral enzyme called reverse
transcriptase. The viral DNA copy is then integrated into the host
chromosome where it exists in a latent state, similar to the herpesviruses.
Reactivation and replication require a reversal of the entire process. Some
retroviruses lyse the host cell during the process of replication. In the case
of HIV, the infected cells regulate the immunologic defense system of the host,
and their lysis leads to a permanent suppression of the immune response.
In
addition to causing infectious diseases, certain viruses also have the ability
to transform normal host cells into malignant cells during the replication
cycle. This group of viruses is referred to as oncogenic and includes certain
retroviruses and DNA viruses, such as the herpesviruses, adenoviruses, and
papovaviruses. Human papillomaviruses (HPVs), members of the papovavirus
family, cause cutaneous and genital warts, and several genotypes are associated
with cervical cancer. The first vaccine (Gardasil) to prevent cervical cancer,
precancerous genital lesions, genital warts, and anal and oropharyngeal cancers
due to HPV types 6, 11, 16, and 18 was developed in 2006.
Bacteria
Bacteria
are autonomously replicating unicellular organisms known as prokaryotes because
they lack an organized nucleus. Compared with nucleated eukaryotic cells, the
bacterial cell is small and structurally relatively primitive. Similar to
eukaryotic cells, but unlike viruses, bacteria contain both DNA and RNA. They
are the smallest of all living cells and range from 0.1 to 10 µm. They contain no organized
intracellular organelles, and the genome consists of only a single chromosome
of DNA. Many bacteria transiently harbor smaller extrachromosomal pieces of
circular DNA called plasmids. Occasionally, plasmids contain genetic
information that increases the virulence or antibiotic resistance of the
organism.
The
prokaryotic cell is organized into an internal compartment called the cytoplasm,
which contains the reproductive and metabolic machinery of the cell. The
cytoplasm is surrounded by a flexible lipid membrane, called the cytoplasmic
membrane. This in turn is enclosed within a rigid cell wall. The structure
and synthesis of the cell wall determine the microscopic shape of the bacterium
(e.g., spherical [cocci],
helical
[spirilla], or elongate [bacilli]). Most bacteria produce a cell wall composed of a distinctive polymer known as peptidoglycan. This polymer is
produced only by prokaryotes and is therefore an attractive target for
antibacterial therapy. Several bacteria synthesize an extracellular capsule
composed of protein or carbohydrate. The capsule protects the organism from
environmental hazards such as the immunologic defenses of the host.
Certain
bacteria are motile as the result of external whiplike appendages called flagella.
The flagella rotate like a propeller, transporting the organism through a
liquid environment. Bacteria can also produce hairlike structures projecting
from the cell surface called pili or fimbriae, which enable the organism
to adhere to surfaces such as mucous membranes or other bacteria.
Most
prokaryotes reproduce asexually by simple cellular division. The manner in
which an organism divides can influence the microscopic morphology. For
instance, when the cocci divide in chains, they are called streptococci;
in pairs, diplococci; and in clusters, staphylococci. The growth
rate of bacteria varies significantly among different species and depends
greatly on physical growth conditions and the availability of nutrients. In the
laboratory, a single bacterium placed in a suitable growth environment, such as
an agar plate, reproduces to the extent that it forms a visible colony com-
posed of millions of bacteria within a few hours (Fig. 12.5).
In
nature, however, bacteria rarely exist as single cells floating in an aqueous
environment. Rather, bacteria prefer to stick to and colonize environmental
surfaces, producing structured communities called biofilms. The
organization and structure of biofilms permit access to available nutrients and
elimination of metabolic waste. Within the biofilm, individual organisms use
chemical signaling as a form of primitive intercellular communication to
represent the state of the environment. These signals inform members of the
community when sufficient nutrients are available for proliferation or when
environmental conditions warrant dormancy or evacuation. Examples of biofilms abound in nature and are found on surfaces
of aquatic environments and on
humans. Eighty percent of all chronic infections are due to the presence of
biofilms.
The
physical appearance of a colony of bacteria grown on an agar plate can be quite
distinctive for different species. Bacteria are also identified according to
how they divide. Some bacteria produce pigments that give colonies a unique
color; some produce highly resistant spores when faced with an unfavorable
environment. The spores can exist in a quiescent state almost indefinitely
until suitable growth conditions are encountered, at which time the spores
germinate and the organism resumes normal metabolism and replication.
Bacteria
are extremely adaptable life forms. They are found not just in humans and other
hosts but in almost every environ- mental extreme on earth. However, each
individual bacterial species has a well-defined set of growth parameters,
including nutrition, temperature, light, humidity, and atmosphere. Bacteria
with extremely strict growth requirements are called fastidious. For
example, Neisseria gonorrhoeae, the bacterium that causes gonorrhea,
cannot live for extended periods outside the human body. Some bacteria require
oxygen for growth and metabolism and are called aerobes. Others cannot
survive in an oxygen-containing environment and are called anaerobes. An
organism capable of adapting its metabolism to aerobic or anaerobic conditions
is called facultatively anaerobic.
In the
laboratory, bacteria are generally classified according to the microscopic
appearance and staining properties of the cell. The Gram stain is the most
widely used staining procedure. Bacteria are designated as gram-positive organisms
if they are stained purple by a primary basic dye (usually crystal violet).
Those that are not stained by the crystal violet but are counterstained red by
a second dye (safranin) are called gram-negative organisms. Staining
characteristics and microscopic morphology are used in combination to describe
bacteria. For example, Streptococcus pyogenes, the agent of scarlet
fever and rheumatic fever, is a gram-positive streptococcal organism that is spherical, grows in chains, and stains
purple by Gram stain. Legionella
pneumophila, the bacterium responsible for Legionnaire disease, is a
gram-negative rod.
Another
means of classifying bacteria according to microscopic staining properties is
the acid-fast stain. Because of their unique cell membrane fatty acid
content and composition, certain bacteria are resistant to the decolorization
of a primary stain (either carbol fuchsin or a combination of auramine and
rhodamine) when treated with a solution of acid alcohol. These organisms are
termed acid-fast and include a number of significant human pathogens,
most notably Mycobacterium tuberculosis and other mycobacteria.
For
purposes of taxonomy (i.e., identification and classification), each
member of the bacterial kingdom is categorized into a small group of
biochemically and genetically related organisms called the genus and
further subdivided into distinct individuals within the genus called species.
The genus and species assignment of the organism is reflected in its name (e.g.,
Staphylococcus [genus] aureus [species]).
Spirochetes. The spirochetes are
an eccentric category of bacteria that are mentioned separately because of
their unusual cellular morphology and distinctive mechanism of motility.
Technically, the spirochetes are gram-negative rods but are unique in that the
cell’s shape is helical and the length of the organism is many times its width.
A series of filaments are wound about the cell wall and extend the entire
length of the cell. These filaments propel the organism through an aqueous
environment in a corkscrew motion.
Spirochetes
are anaerobic organisms and comprise three genera: Leptospira, Borrelia,
and Treponema. Each genus has saprophytic and pathogenic strains. The
pathogenic leptospires infect a wide variety of wild and domestic animals.
Infected animals shed the organisms into the environment through the urinary
tract. Transmission to humans occurs by contact with infected animals or
urine-contaminated surroundings. Leptospires gain access to the host directly
through mucous membranes or breaks in the skin and can produce a severe and
potentially fatal illness called Weil syndrome. In contrast, the
borreliae are transmitted from infected animals to humans through the bite of
an arthropod vector such as lice or ticks. Included in the genus Borrelia are
the agents of relapsing fever (Borrelia recurrentis)
and Lyme disease (B. burgdorferi).
Pathogenic
Treponema species require no intermediates and
are spread from person to person by direct contact. The most important member
of the genus is Treponema pallidum, the causative agent of syphilis.
Mycoplasmas. The mycoplasmas are
unicellular prokaryotes capable of independent replication. These organisms are
less than one third the size of bacteria at approximately 0.3 µm at their
largest diameter and contain a small DNA genome approximately one half the size
of the bacterial chromosome. The cell is composed of cytoplasm surrounded by a
membrane but, unlike bacteria, the mycoplasmas do not produce a rigid
peptidoglycan cell wall. As a consequence, the microscopic appearance of the
cell is highly variable, ranging from coccoid forms to filaments, and the
mycoplasmas are resistant to cell-wall–inhibiting antibiotics, such as
penicillins and cephalosporins.
The
mycoplasmas affecting humans are divided into three genera: Mycoplasma, Ureaplasma,
and Acholeplasma. The first two require cholesterol from the environment
to produce the cell membrane; the acholeplasmas do not. In the human host,
mycoplasmas are commensals. However, a number of species are capable of
producing serious diseases, including pneumonia (Mycoplasma pneumoniae),
genital infections (Mycoplasma hominis and Ureaplasma urealyticum),
and maternally transmitted respiratory infections to infants with low birth weight (U. urealyticum). not produce disease in the cells of certain
arthropods such as fleas, ticks, and
lice. The organisms are accidentally transmitted to humans through the bite of
the arthropod (i.e., the vector) and produce a number of potentially
lethal diseases, including Rocky Mountain spotted fever and epidemic typhus.
Rocky Mountain spotted fever is a reportable disease that has increased in
frequency over the last decade from two cases in 1 million people to eight
cases in 1 million people. However, the death rate has decreased to
approximately 0.5%.
The Chlamydiaceae
are slightly smaller than the Rickettsiaceae but are structurally
similar and are transmitted directly between susceptible vertebrates without an
intermediate arthropod host. Transmission and replication of Chlamydiaceae occur
through a defined life cycle. The infectious form, called an elementary body,
attaches to and enters the host cell, where it transforms into a larger reticulate
body. This undergoes active replication into multiple elementary bodies,
which are then shed into the extracellular environment to initiate another
infectious cycle. Chlamydial diseases of humans include sexually transmitted
genital infections (Chlamydophila trachomatis), which are the most
common of the bacterial sexually transmitted infections (STIs)10; ocular
infections and pneumonia of newborns (C. trachomatis); upper and lower
respiratory tract infections in children, adolescents, and young adults (Chlamydophila
pneumoniae), which generally does not cause severe disease unless there is
an underlying pulmonary disorder2; and respiratory disease acquired from
infected birds (Chlamydia psittaci).
Organisms
within the family Anaplasmataceae (including the reorganized genera Ehrlichia,
Anaplasma, Neorickettsia, and Wolbachia) are also obligate
intracellular organisms that resemble the Rickettsiaceae in structure
and produce a variety of veterinary and human diseases, some of which have a
tick vector. These organisms target host mononuclear and polymorphonuclear
white blood cells for infection and, similar to the Chlamydiaceae,
multiply in the cytoplasm of infected leukocytes within vacuoles called morulae.
Unlike the Chlamydiaceae, however, the Anaplasmataceae do not
have a defined life cycle and are independent of the host cell for energy
production. Ehrlichia sennetsu, which is primarily restricted to Japan,
produces a disease called sennetsu fever that resembles IM. Disease
caused by this organism differs from other Anaplasmataceae because it is
associated with eating raw fish infested with E. sennetsu–infected
parasites. The most common infections caused by Anaplasmataceae are
human monocytic and granulocytic ehrlichiosis. Human monocytic ehrlichi-osis is
a disease caused by Ehrlichia chaffeensis and E. canis that can
easily be confused with Rocky Mountain spotted fever.
Clinical
disease severity ranges from mild to life threatening. Manifestations include
generalized malaise, anorexia and nausea, fever, and headache. Decreases in
white blood cells (leukopenia) and platelets (thrombocytopenia) often occur.
Severe sequelae include severe respiratory failure, encephalopathy, and acute
renal failure. The disease is usually more severe in older adults and people
with compromised immune function. Evidence
validates the importance
of empirical antibiotic treatment when one suspects ehrlichiosis
since a fulminant and
life-threatening infection is likely with immu- nocompromised people. Human
granulocytic ehrlichiosis, which is caused by two species (Anaplasma
phagocytophilum and Ehrlichia ewingii), is also transmitted by
ticks. The symptoms are similar to those seen with human monocytotropic
ehrlichiosis.
The genus
Coxiella contains only one species, C. burnetii. Like its
rickettsial counterparts, it is a gram-negative intracellular organism that
infects a variety of animals, including cattle, sheep, and goats. In humans, Coxiella
infection produces a disease called Q fever, characterized by a nonspecific
febrile illness often accompanied by headache, chills, and mild pneumonia-like
symptoms. The organism produces a highly resistant sporelike stage that is
transmitted to humans when contaminated animal tissue is aerosolized (e.g., during
meat processing) or by ingestion of contaminated milk.
Fungi
The fungi
are free-living, eukaryotic
saprophytes found in every
habitat on earth. Some are members of the normal human microflora. Fortunately,
few fungi are capable of causing diseases in humans, and most of these are
incidental, self-limited infections of skin and subcutaneous tissue. Serious
fungal infections are rare and usually initiated through puncture wounds or
inhalation. Despite their normally harmless nature, fungi can cause
life-threatening opportunistic diseases when host defense capabilities have
been disabled.
The fungi
can be separated into two groups, yeasts and molds, based on rudimentary
differences in their morphology. The yeasts are single-celled organisms,
approximately the size of red blood cells, which reproduce by a budding
process. The buds separate from the parent cell and mature into identical
daughter cells. Molds produce long, hollow, branching filaments called hyphae.
Some molds produce cross walls, which segregate the hyphae into compartments,
and others do not. A limited number of fungi are capable of growing as yeasts
at one temperature and as molds at another. These organisms are called dimorphic
fungi and include a number of human pathogens such as the agents of
blastomycosis (Blastomyces dermatitidis), histoplasmosis (Histoplasma
capsulatum), and coccidioidomycosis (Coccidioides immitis).
The
appearance of a fungal colony tends to reflect its cellular composition.
Colonies of yeast are generally smooth with a waxy or creamy texture. Molds
tend to produce cottony or powdery colonies composed of mats of hyphae
collectively called a mycelium. The mycelium can penetrate the growth
surface or project above the colony like the roots and branches of a tree.
Yeasts and molds produce a rigid cell wall layer that is chemically unrelated
to the peptidoglycan of bacteria and is therefore not susceptible to the
effects of penicillin-like antibiotics.
Most
fungi are capable of sexual or asexual reproduction. The former process
involves the fusion of zygotes with the production of a recombinant zygospore.
Asexual reproduction involves the formation
of highly resistant
spores called conidia or sporangiospores, which are borne by
specialized structures
that arise from the hyphae. Molds are identified inthe laboratory by the
characteristic microscopic appearance of the asexual fruiting structures and
spores.
Like the
bacterial pathogens of humans, fungi can produce disease in the human host only
if they can grow at the temperature of the infected body site. For example, a
number of fungal pathogens called dermatophytes are incapable of growing
at core body temperature (37°C), and the infection is limited to the cooler
cutaneous surfaces. Diseases caused by these organisms, including ringworm,
athlete’s foot, and jock itch, are collectively called superficial mycoses.
Systemic mycoses are serious fungal infections of deep tissues and, by
definition, are caused by organisms capable of growth at 37°C. Yeasts such as Candida
albicans are commensal flora of the skin, mucous membranes, and
gastrointestinal tract and are capable of growth at a wider range of
temperatures. Intact immune mechanisms and competition for nutrients provided
by the bacterial flora normally keep colonizing fungi in check. Alterations in
either of these components by disease states or antibiotic therapy can upset
the balance, permitting fungal overgrowth and setting the stage for
opportunistic infections.
Parasites
In a
strict sense, any organism that derives benefits from its biologic relationship
with another organism is a parasite. In the study of clinical microbiology,
however, the term parasite has evolved to designate members of the
animal kingdom that infect and cause disease in other animals, and includes protozoa,
helminths, and arthropods.
The
protozoa are unicellular animals with a complete complement of eukaryotic
cellular machinery, including a well-defined nucleus and organelles.
Reproduction may be sexual or asexual, and life cycles may be simple or
complicated, with several maturation stages requiring more than one host for
completion. Most are saprophytes, but a few have adapted to the accommodations
of the human environment and produce a variety of diseases, including malaria,
amebic dysentery, and giardiasis.2 Protozoan infections can be passed directly
from host to host such as through sexual contact, indirectly through
contaminated water or food, or by way of an arthropod vector. Direct or
indirect transmission results from the ingestion of highly resistant cysts or
spores that are shed in the feces of an infected host. When the cysts reach the
intestine, they mature into vegetative forms called trophozoites, which
are capable of asexual reproduction or cyst formation. Most trophozoites are
motile by means of flagella, cilia, or ameboid motion.
The
helminths are a collection of wormlike parasites that include the nematodes or
roundworms, cestodes or tapeworms, and trematodes or flukes. The helminths reproduce
sexually within the definitive host, and some require an intermediate host for
the development and maturation of offspring. Humans can serve as the definitive
or intermediate host and, in certain diseases such as trichinosis, as both.
Transmission of helminth diseases occurs primarily through the ingestion of
fertilized eggs (ova) or the penetration of infectious
larval stages through the skin directly or with the aid of an arthropod vector. Helminth infections can
involve many organ systems
and sites, including the liver and lung, urinary and intestinal tracts,
circulatory and central nervous systems, and muscle. Although most helminth
diseases have been eradicated from the United States, they are still a major
health concern of developing nations.
The
parasitic arthropods of humans and animals include the vectors of infectious
diseases (e.g., ticks, mosquitoes, biting flies) and the ectoparasites.
The ectoparasites infest external body surfaces and cause localized tissue
damage or inflammation secondary to the bite or burrowing action of the
arthropod. The most prominent human ectoparasites are mites (scabies),
chiggers, lice (head, body, and pubic), and fleas. Transmission of
ectoparasites occurs directly by contact with immature or mature forms of the
arthropod or its eggs found on the infested host or the host’s clothing,
bedding, or grooming articles such as combs and brushes. Many of the
ectoparasites are vectors of other infectious diseases, including endemic
typhus and bubonic plague (fleas) and epidemic typhus (lice).